You may be responding to invisible environmental stressors when your body shows persistent headaches, unexplained fatigue, respiratory irritation or shortness of breath, skin reactions or rashes, disrupted sleep or heightened anxiety, and brain fog or concentration problems. Recognizing these six signs helps you take targeted steps-air quality, allergens, chemicals, or electromagnetic exposure-to protect your health and seek appropriate testing or mitigation.
Understanding invisible environmental stressors
Common types (air pollutants, VOCs, mold, EMFs, noise, indoor allergens)
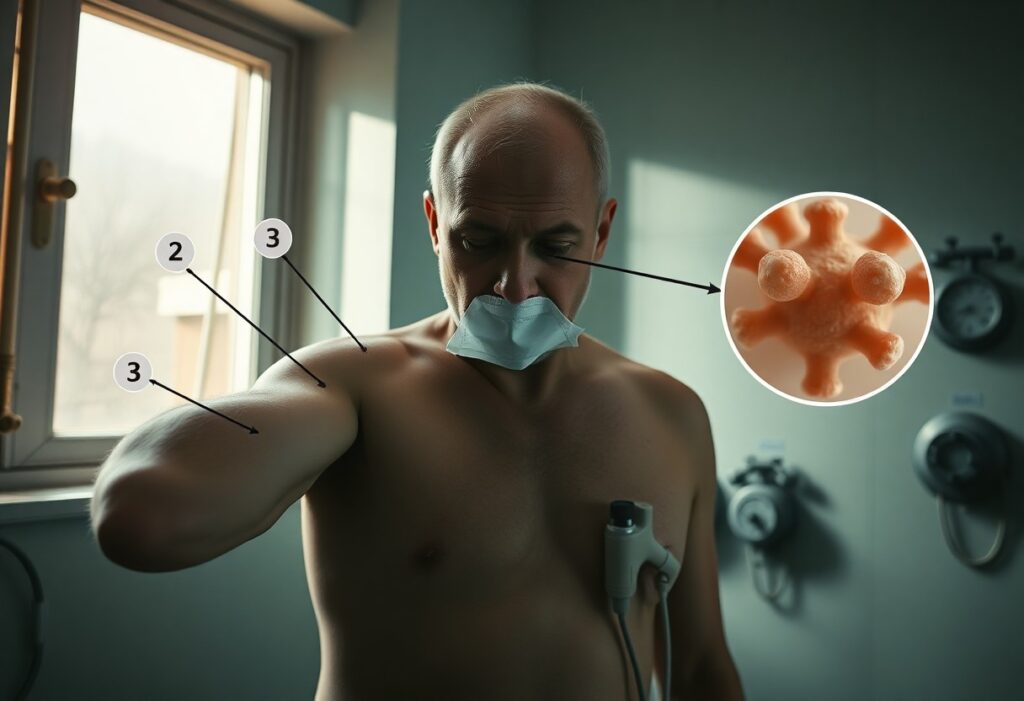
You routinely encounter fine particulates (PM2.5/PM10) and gases from traffic and combustion, volatile organic compounds from paints and cleaners, mold spores in damp buildings, low-frequency EMFs from wiring and devices, persistent noise above 55-65 dB, and indoor allergens like dust mite and pet dander. Short-term spikes in PM2.5 or VOCs often trigger headaches and irritation, while mold and allergens provoke asthma and rhinitis. Knowing how these sources overlap helps you target mitigation.
- Air pollutants: PM2.5, NO2, ozone
- VOCs: formaldehyde, benzene, toluene
- Mold: Stachybotrys, Aspergillus in damp areas
- EMFs: high-voltage lines, wiring, routers
- Noise & indoor allergens: traffic/HVAC noise; dust mites, pet dander
| Air pollutants (PM2.5, NO2, O3) | Raise systemic inflammation (CRP, IL-6), trigger asthma exacerbations and increase cardiopulmonary admissions; WHO PM2.5 annual guideline is 5 µg/m³. |
| VOCs (formaldehyde, benzene) | Cause mucosal irritation and headaches; off-gassing from new furniture/building materials can drive indoor levels into low-ppb-high-ppb ranges. |
| Mold | Leads to allergic disease, chronic sinusitis and asthma flares; visible dampness and musty odors commonly indicate elevated spore counts. |
| EMFs | Associated with sleep disruption and headaches in some reports; biological effects vary with frequency, intensity and chronicity of exposure. |
| Noise & indoor allergens | Chronic noise >55 dB elevates stress hormones; dust mites and pet dander drive IgE-mediated allergic inflammation and airway hyperresponsiveness. |
How invisible stressors affect the body (inflammation, HPA-axis activation, oxidative stress)
You develop immune activation when inhaled irritants and allergens elevate pro-inflammatory cytokines (IL-6, TNF-α) and C-reactive protein, while repeated exposure stimulates the HPA axis, raising cortisol and disrupting sleep and metabolic control. Oxidative stress follows as reactive oxygen species rise and glutathione is consumed, contributing to endothelial dysfunction and neuroinflammation. Small, repeated insults-like daily PM2.5 exposure or ongoing VOC off-gassing-accumulate and increase cardiometabolic and respiratory risk.
In clinical and population studies, short-term PM2.5 spikes correlate with acute increases in inflammatory markers and hospital admissions for heart attacks and asthma, while long-term exposure is linked to higher baseline CRP and accelerated atherosclerosis. You may notice symptom patterns: headaches and concentration problems during VOC peaks, worse asthma after damp-season mold growth, or persistent fatigue with chronic noise and sleep loss-each reflecting overlapping inflammatory, neuroendocrine, and oxidative pathways that compound over time.
The 6 critical signs your body is reacting
You’ll usually see patterns, not single events: persistent fatigue, cognitive fog, recurrent headaches, respiratory irritation, disrupted sleep, and new allergic or inflammatory reactions. Each sign may appear gradually over weeks to months and often worsens in specific places (office, home, commute). For example, people exposed to poor indoor air or new building materials report symptom clusters within 2-12 weeks, and tracking timing against locations helps identify the invisible trigger.
Persistent unexplained fatigue and reduced stamina
You may find tasks that were easy now drain you: climbing stairs leaves you winded, workouts feel harder, and you need more recovery time. Fatigue from environmental stressors often persists despite adequate sleep and nutrition, and can reduce daily activity by 20-40% compared with your baseline, pushing you to cut back on hobbies or work hours without an obvious medical cause.
Cognitive fog, difficulty concentrating and memory lapses
You’ll notice trouble focusing, slower decision-making, and forgetting appointments or names. These changes can be subtle-errors at work, reading without retention, or repeated mental fatigue after brief tasks-and often correlate with time spent in a specific environment where symptoms reliably worsen.
Mechanisms include elevated indoor CO2 (>1,000 ppm), volatile organic compounds (VOCs), and inflammatory cytokines; research links such exposures to measurable declines in attention and decision-making (often a 5-10% performance drop on neurocognitive tests). Simple monitoring of CO2 and VOC spikes during the day can reveal clear correlations with your symptom pattern.
Frequent headaches, light/sound sensitivity or migraines
You might experience recurring tension-type headaches or migraine attacks triggered by odors, bright lights, or noise in particular environments. Sensitivity often manifests as increased frequency or intensity of headaches when you’re at work, in a newly renovated space, or after exposure to cleaning chemicals or strong fragrances.
Chemical triggers (solvents, fragrances) can activate trigeminal pathways and promote neurogenic inflammation; surveys show a large subgroup of migraine sufferers identify odors as triggers. Tracking headache onset against exposure events, and noting accompanying autonomic signs (nausea, photophobia), helps isolate environmental contributors for targeted mitigation.
Respiratory irritation, chronic sinus symptoms or new cough
You may develop persistent nasal congestion, postnasal drip, chronic throat clearing, or a new nonproductive cough that flares in certain buildings. Symptoms often mimic allergic rhinitis or low-grade asthma and can persist for weeks after exposure, worsening with dampness, visible mold, or combustion-related pollutants.
Common culprits include mold spores, dust-mite reservoirs, NO2 from gas appliances, and fine particulates; sensitive people can show reduced peak expiratory flow or increased bronchial hyperreactivity when exposed. Objective testing-spirometry, peak flow diaries, and nasal cytology-can document exposure-linked changes and guide remediation.
Sleep disturbances, nonrestorative sleep or shifted circadian rhythm
Your sleep may fragment, feel nonrestorative, or shift earlier/later without behavioral change, often linked to nighttime light, noise, or ongoing low-grade chemical exposures. Daytime fatigue, heightened irritability, and impaired recovery after sleep are common, especially when symptoms intensify in one location.
Light at night (blue-rich sources) and nocturnal noise increase sleep fragmentation and reduce deep and REM sleep; some indoor pollutants can suppress melatonin. Monitoring bedroom light levels, noise patterns, and using actigraphy or sleep diaries often shows clear associations between environmental disturbances and altered sleep architecture.
New-onset allergies, skin reactions or unexplained inflammation
You may suddenly develop itchy rashes, contact dermatitis, hives, or localized swelling after exposure to new products, building materials, or airborne irritants. Symptoms can appear days to weeks after introduction of a fragrance, preservative, or construction material and often localize to exposed skin or respiratory mucosa.
Patch testing, serum IgE, and clinical history frequently identify agents like formaldehyde, fragrances, parabens, or certain metal salts; case reports often link workplace outbreaks (new carpeting, adhesives) to clusters of dermatitis. Documenting product changes and spatial patterns helps clinicians confirm allergic versus irritant or inflammatory causes.
Assessing exposure and personal risk
Gauge your risk by combining exposure intensity, duration and personal susceptibility. You should compare measured or estimated levels against standards – for example WHO’s PM2.5 annual guideline of 5 µg/m3 or occupational 8‑hour TWA limits from OSHA/NIOSH – and factor in age, pregnancy, asthma or immune compromise. Short high‑concentration spikes can matter more than low chronic levels; track frequency, duration and any symptom patterns tied to specific environments to estimate your cumulative burden.
Spotting likely sources at home, work and commute
At home, you should check gas stoves, unvented heaters, recent renovations (fresh paint, new cabinetry releasing VOCs) and water‑damaged areas where mold prefers humidity above ~60%. At work, inspect printers, solvent storage and confined equipment rooms with poor ventilation. During commute, diesel exhaust from buses and idling traffic often spikes your PM exposure. If your basement sits over uranium‑rich soil, radon can exceed the EPA action level of 4 pCi/L, so test accordingly.
Practical screening tools and when to escalate to professional testing
You can start with inexpensive tools: home radon kits ($15-$40), plug‑in PM2.5/CO2 monitors ($100-$300) and battery CO alarms, while DIY mold or VOC kits offer only rough signals. Escalate to a certified industrial hygienist or accredited lab when you detect repeated exceedances, persistent unexplained symptoms among household members or coworkers, or complex chemical mixtures that require sorbent tubes and GC‑MS for accurate quantification.
If your short tests show radon above 4 pCi/L or CO peaks approaching the EPA 8‑hour guideline of ~9 ppm, pursue follow‑up measurement and mitigation. For VOCs and formaldehyde, passive sorbent badges with 24-72‑hour sampling sent to an accredited lab yield actionable concentrations; remediation decisions typically rely on GC‑MS reports. You should involve industrial hygienists for workplace sampling plans and homeowners should hire certified radon mitigators or licensed mold remediators based on professional findings.
Reducing exposure and strengthening resilience
Environmental interventions (ventilation, filtration, material choices)
Increase ventilation to lower pollutant buildup and, where possible, aim for 4-6 air changes per hour in high-occupancy rooms; you can also boost outdoor air fractions in your HVAC. Upgrade to MERV‑13 or higher and add portable HEPA cleaners (HEPA traps 99.97% of ≥0.3 µm particles and can cut indoor PM2.5 by up to ~80%). Choose low‑VOC paints (<50 g/L), avoid particleboard, and select GREENGUARD‑certified or EPD-labeled materials to reduce off‑gassing.
Lifestyle and supportive medical measures (sleep, nutrition, stress management)
Prioritize 7-9 hours of consistent sleep and a 150-minute weekly exercise goal to lower systemic inflammation; you’ll see benefits in energy and symptom tolerance. Follow a Mediterranean-style, anti-inflammatory diet-oily fish twice weekly, 25-30 g fiber/day, reduce ultra-processed foods-and consider 1-2 g combined EPA/DHA or 1,000-2,000 IU vitamin D after testing. Add 10 minutes daily breathing or an 8-week mindfulness program and consult your clinician for targeted allergy or environmental testing.
Improve sleep hygiene by keeping your bedroom cool (60-67°F), dark, and screen-free 30-60 minutes before bed, and use short naps (<20 minutes) if needed. For nutrition specifics, you can aim for oily fish servings twice weekly, 25-30 g fiber, and limit trans fats; supplementation (vitamin D to >30 ng/mL, omega‑3s) should follow a provider’s advice. Combine nasal saline, HEPA bedroom filtration, allergen-proof bedding, and pursue referral to environmental or occupational medicine if symptoms persist despite these measures.
When to seek medical or occupational evaluation
If symptoms persist beyond two weeks despite reducing exposure, or if multiple coworkers report similar complaints within 48 hours, you should pursue formal evaluation; examples include persistent cough, recurrent headaches, new cognitive fog interfering with work, or abnormal pulse oximetry (<92%). Contact occupational health for suspected lead, asbestos, solvent, or pesticide exposure, and seek urgent care for chest pain, syncope, or sudden neurologic changes. Early reporting helps trigger exposure assessment and targeted testing.
Red flags that require prompt clinical assessment or specialist referral
If you experience severe or worsening shortness of breath, chest pain, syncope, hemoptysis, new focal neurologic deficits, or oxygen saturation under 92%, seek immediate clinical assessment. Also get urgent review for high fevers (>38.5°C for >48 hours), unexplained weight loss >10% in six months, or progressive functional decline that prevents work. Multiple affected coworkers or acute symptom clusters after a single event (chemical spill, gas leak) warrant rapid specialist referral.
Common diagnostic pathways and tests clinicians use
Clinicians start with a focused exposure history and physical exam, then order targeted tests: spirometry (pre/post bronchodilator with >12% FEV1 change significant), chest X‑ray or HRCT, CBC with differential (eosinophils >500/µL suggest eosinophilic processes), basic metabolic panel, ESR/CRP, pulse oximetry/ABG if hypoxic, blood lead level (CDC reference >5 µg/dL in children), urinary pesticide metabolites, and specific serologies or skin patch tests for suspected allergens.
When initial tests are non-diagnostic, workflow often escalates: occupational hygiene conducts air or surface sampling (PM2.5 in µg/m3, VOCs in ppm) and personal sampling per NIOSH methods, specialists may add bronchoscopy with BAL, HRCT pattern analysis, neuropsychological batteries for cognitive complaints, or repeat biomonitoring after exposure cessation to document trends. Results guide mitigation, workplace controls, and compensation decisions.
Practical resources and monitoring
You’re advised to use layered monitoring: continuous PM2.5 sensors (PurpleAir/IQAir), CO2 meters for ventilation (Aranet4), and long‑term radon tests (Airthings or mailed kits). Target PM2.5 under 12 µg/m3 annual (24‑hr <35 µg/m3) and CO2 <1000 ppm. Export time‑stamped logs, pair readings with symptom entries, and take photos of sources or HVAC settings so you can present clear, dated evidence when requesting investigation or remediation.
Recommended consumer monitors, checklists and symptom logs
You should combine a PurpleAir or IQAir for PM2.5, Aranet4 (or similar) for CO2, and Airthings for radon/TVOCs; add a handheld VOC/formaldehyde meter for suspect materials. Use a daily checklist with location, device reading, HVAC/occupancy status, and recent activities. Log symptoms with date/time, severity (1-10), and suspected triggers. Store everything in a spreadsheet or apps like AirVisual so trends, spikes and correlations are easy to export for specialists or landlords.
Workplace/tenant rights, reporting channels and further reliable reading
You can file workplace complaints to OSHA (1‑800‑321‑6742) or raise issues through your employer’s safety committee; tenants should submit written complaints to building management, then to local code enforcement or the health department. EPA and state radon programs offer testing guidance, while HUD covers federally assisted housing. Keep copies of all communications, photos and monitor logs to strengthen requests for inspections, temporary relocation or formal remediation.
Document methodically: export CSVs from monitors, take date‑stamped photos, collect symptom logs and witness statements. Send a written complaint (email plus certified mail) and allow a remediation window-commonly 7-14 days-then escalate to local health/code offices or OSHA with your packet. Consider hiring a Certified Industrial Hygienist for a formal report; IH findings often prompt faster landlord or employer action. Contact legal aid or tenant advocacy groups for help with leases, housing court or relocation claims.
Conclusion
To wrap up, stay alert to subtle cues-sleep disruption, persistent headaches, digestive changes, skin flare-ups, heightened sensitivity, and unexplained fatigue-because these signs show how environmental stressors affect your body. Take proactive steps to identify sources, adjust your surroundings, and consult professionals so you can reduce exposure and restore balance to your health.