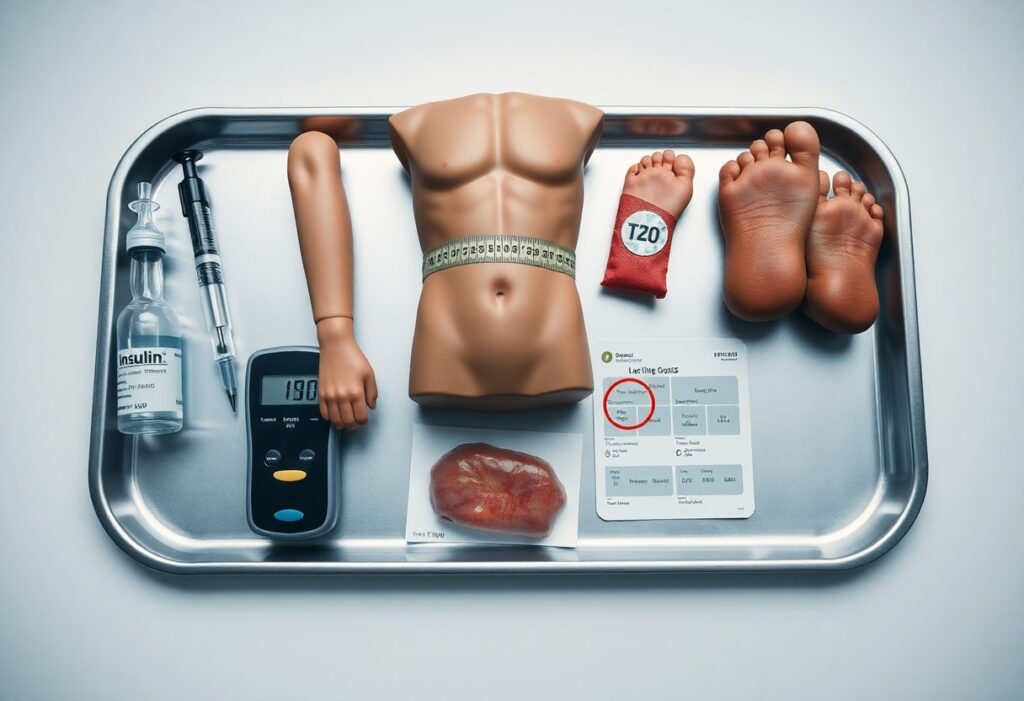
With insulin central to energy balance and tissue repair, you may overlook subtle signs that your metabolic signals are misfiring; this post guides you through seven hidden indicators-fatigue despite sleep, unexplained weight changes, persistent cravings, slowed wound healing, brain fog, frequent infections, and fluctuating mood-so you can identify disruptions early, understand their implications for your energy and recovery, and take informed steps to restore metabolic resilience.
Key Takeaways:
- Persistent daytime fatigue and post-meal energy crashes indicate impaired glucose uptake that limits cellular fuel and repair.
- Strong cravings for sugar or frequent snacking reflect disrupted hunger signals and blood-sugar instability driven by insulin dysregulation.
- Unexplained abdominal weight gain or difficulty losing belly fat signals altered insulin action promoting visceral fat storage.
- Slow wound healing, recurrent infections, or skin changes (e.g., darkened creases) point to compromised tissue repair and immune response.
- Brain fog, poor concentration, or mood swings arise from fluctuating glucose availability and impaired brain energy metabolism.
- Sleep problems or excessive daytime sleepiness can result from metabolic-hormone imbalance that disrupts restorative processes.
- Elevated triglycerides, low HDL, or high blood pressure are metabolic markers that often accompany insulin-related dysfunction and increase cardiovascular risk.
Understanding Insulin and Metabolic Signals
You experience insulin as the switch that tells cells whether to burn fuel or store it; when signaling is balanced you run efficient glucose uptake, stable energy, and periodic repair cycles like autophagy during fasting windows of 12-16+ hours. Disturbances flip priority toward storage, elevate fasting insulin, and blunt repair processes, so small changes in meal composition, activity, or sleep quickly shift how your body allocates energy and resources.
The Role of Insulin in Energy Regulation
You rely on insulin to move glucose into muscle and adipose via GLUT4 translocation, suppress hepatic gluconeogenesis, and promote glycogen synthesis; insulin rises within 10-15 minutes of a carbohydrate load and typically peaks 30-60 minutes, with a plasma half-life around 4-6 minutes. Clinically, fasting insulin often sits between ~2-20 µU/mL, and exaggerated postprandial spikes signal inefficient energy handling.
Factors Affecting Insulin Sensitivity
You can shift sensitivity rapidly: a single 30-60 minute bout of moderate exercise improves GLUT4 activity for 24-48 hours, while increased visceral fat and waist circumferences (>102 cm men, >88 cm women) strongly associate with worse insulin response. Sleep under 6 hours, chronic cortisol elevation, diets high in refined carbs or saturated fats, certain meds (systemic steroids), age, and genetics all modulate how your tissues respond to insulin.
- Physical activity – 30 minutes of brisk walking or interval work boosts insulin-mediated glucose disposal for up to 48 hours.
- Visceral adiposity – central fat secretes inflammatory cytokines (IL-6, TNF-α) that impair insulin signaling.
- Sleep and stress – less than 6 hours or chronic cortisol exposure raises fasting insulin and blunts postprandial clearance.
- The gut microbiome – low diversity or dysbiosis correlates with higher insulin resistance via metabolites like LPS and altered bile acids.
You can leverage interventions that show measurable change: in the Diabetes Prevention Program a 7% weight loss cut progression to type 2 diabetes by ~58%, and exercise interventions commonly lower HOMA‑IR by 10-30% within 8-12 weeks. Dietary shifts toward higher fiber, monounsaturated fats, and reduced refined carbs produce rapid postprandial insulin reductions, while consistent resistance training builds muscle mass that increases baseline glucose uptake.
- Prioritize combined aerobic and resistance training at least 3-5 times weekly to sustain insulin sensitivity gains.
- Aim for 7-9 hours of sleep and stress-reduction practices to limit cortisol-driven insulin resistance.
- Choose high-fiber whole foods, olive oil, nuts, and limit refined sugars to blunt postprandial spikes.
- The Mediterranean-style dietary pattern and modest weight loss both show reproducible improvements in insulin sensitivity in randomized trials.
Hidden Signs of Disrupted Metabolic Signals
Symptoms often surface long before a diagnosis: you may see post-meal glucose spikes (>140 mg/dL at 2 hours) or fasting insulin creeping above ~10-15 μIU/mL, afternoon energy crashes 2-4 hours after carbs, increased hunger despite adequate calories, and slower wound or muscle healing. These patterns, combined with unexplained blood pressure or lipid changes, point to insulin signaling that is misdirecting fuel use and repair, even if weight and A1c look borderline.
Unexplained Fatigue and Low Energy Levels
When insulin-driven glucose uptake falters, your cells get less fuel and you feel foggy or exhausted-commonly 2-4 hours after a carb-rich meal. You might notice daytime sleepiness despite 7-8 hours of sleep, reduced exercise tolerance, or needing stimulants to get through the afternoon. In clinic, these complaints often correlate with elevated fasting insulin or frequent postprandial glucose excursions on CGM or glucose tolerance testing.
Difficulty in Muscle Repair and Recovery
Insulin normally promotes amino acid uptake and protein synthesis; when signaling is impaired, you experience prolonged soreness and weaker gains after resistance sessions. Instead of recovering in 24-36 hours, your muscle soreness can persist 48-72 hours, strength returns slower, and training adaptations plateau-patterns frequently reported by athletes with metabolic syndrome or older adults with insulin resistance.
Mechanistically, impaired GLUT4 translocation reduces glucose supply to myocytes and blunts insulin-stimulated amino acid transport and mTOR pathway activation, lowering post-exercise muscle protein synthesis observed in tracer studies. Clinically, that shows up as delayed strength recovery, higher perceived exertion on repeat sets, and sometimes persistently elevated inflammatory markers after workouts-signals that your anabolic response to training is being dampened by disrupted insulin signaling.
The Connection Between Insulin and Weight Gain
When your insulin stays elevated, your metabolism favors storage over expenditure: insulin activates lipoprotein lipase and suppresses hormone-sensitive lipase, so excess calories-especially from refined carbs and sugary drinks-are shunted into adipose tissue. Persistent postprandial spikes drive visceral fat accumulation, make hunger signals stronger between meals, and often blunt the impact of calorie restriction, which helps explain why some people struggle to lose weight despite dieting.
The Impact of Insulin Resistance
As your muscle and liver cells become insulin resistant, the pancreas compensates by raising insulin output-often several-fold-creating chronic hyperinsulinemia that further promotes fat storage. You’ll commonly see this pattern paired with increased waist circumference, high triglycerides and low HDL; longitudinal data link higher fasting insulin to greater fat gain over 3-5 years, not just transient weight fluctuations.
Hormonal Imbalances and Weight Management
Insulin interacts with other hormones that govern appetite and fat distribution: leptin, ghrelin, cortisol and sex steroids all shift when insulin signaling is off. For example, up to 10% of reproductive-age women with PCOS experience insulin resistance that amplifies androgen-driven central adiposity, while low testosterone in men correlates with higher visceral fat and worsening insulin sensitivity.
Mechanistically, chronic hyperinsulinemia contributes to leptin resistance so you feel hungry despite ample fat stores, and elevated cortisol from stress favors abdominal fat and gluconeogenesis. Sleep loss and shift work raise evening insulin and ghrelin, increasing caloric intake; addressing these hormonal cross-talks is why weight patterns differ so much between individuals with similar diets.
Dietary Factors Influencing Insulin Levels
Even subtle shifts in what you eat alter insulin dynamics: high-GI carbs provoke rapid spikes while protein and fat blunt responses. Choose lower-GI options-oats (GI ~55), basmati rice (~50), legumes (GI 30-40)-and distribute 20-30 g protein per meal to reduce postprandial peaks. This lets you design meals that stabilize insulin and support repair.
- Refined carbs: white bread, pastries, and many breakfast cereals
- Sugar-sweetened drinks: 12 oz soda ≈ 39 g added sugar
- Ultra-processed snacks: often high in refined fats and simple sugars
- Low-fiber meals: lack the slowing effect on glucose absorption
The Role of Sugar and Processed Foods
Frequent intake of added sugars and processed foods forces repeated insulin surges: WHO guidance recommends keeping added sugars under ~25 g/day, yet a single candy bar or soda can exceed that. You’ll see larger post-meal glucose excursions and clearer insulin resistance signals when diets rely on HFCS and refined starches instead of whole-food alternatives.
Importance of a Balanced Diet
Balancing macronutrients moderates insulin responses-target about 25-30 g fiber daily, 20-30 g protein at each meal, and fats around 25-35% of calories with an emphasis on monounsaturated and omega‑3 sources. You’ll gain steadier energy, fewer glucose spikes (>140 mg/dL at 2 hours), and improved recovery from cellular stress.
Practical swaps produce measurable differences: replacing a sugary breakfast with eggs, veggies, and whole-grain toast reduces 2‑hour glucose excursions, while choosing lentils over white rice can cut postprandial glucose by roughly 20-30% in crossover studies. Prioritize legumes, nuts, fatty fish, whole grains, and leafy greens to blunt insulin peaks and support metabolic repair.
Lifestyle Changes for Better Insulin Sensitivity
Small, consistent shifts in daily habits deliver outsized gains: aim for 150 minutes/week of moderate activity, prioritize whole foods over ultra-processed options, and target 5-10% body-weight loss if you’re overweight to markedly improve insulin action. Reducing added sugars and refined carbs while increasing fiber (25-35 g/day) and lean protein at meals helps blunt postprandial insulin spikes and supports steady energy and repair.
Exercise and Physical Activity
A balanced program combines 150 minutes/week of moderate aerobic activity (or 75 minutes vigorous) with 2-3 resistance sessions to boost muscle glucose uptake; HIIT sessions of 10-20 minutes twice weekly also rapidly improve insulin sensitivity. For example, a 12-week mixed program in adults often shows ~15-25% improvements in insulin responsiveness, so prioritize compound lifts, brisk walking, cycling, and consistent progression.
Sleep and Stress Management
Getting 7-9 hours nightly and keeping a consistent sleep-wake time protects insulin signaling, while chronic stress and elevated cortisol worsen glucose control; practice 5-15 minutes of diaphragmatic breathing, 10-20 minutes of mindfulness, and dim screens an hour before bed to lower evening arousal and support restorative sleep.
Controlled trials show acute sleep restriction (4-5 hours/night for several nights) can reduce insulin sensitivity by roughly 20-30%, and sustained stress elevates cortisol which promotes hepatic glucose production. Implement a fixed wake time, expose yourself to bright morning light, avoid caffeine within six hours of bedtime, use progressive muscle relaxation or guided breathing for 10 minutes before sleep, and consider CBT-I if insomnia persists to restore metabolic balance.
Conclusion
Ultimately you should treat the seven hidden signs as meaningful warnings that insulin dysregulation is sapping your energy and blunting cellular repair; by monitoring symptoms, tracking fasting glucose or HbA1c, improving diet, sleep, and activity, and consulting your clinician you can restore metabolic signals and reclaim sustained energy and recovery.
FAQ
Q: What does persistent low energy or mid-afternoon crashes indicate about my insulin and metabolism?
A: Persistent post-meal fatigue and recurring mid-afternoon energy crashes often reflect unstable blood glucose and impaired insulin signaling. When insulin response is blunted, glucose clearance from the bloodstream is erratic-initial spikes followed by reactive drops-leaving you dependent on stimulants (coffee, sugar) to function. Over time this pattern reduces metabolic flexibility, blunts mitochondrial efficiency, and impairs daytime alertness and physical stamina.
Q: Why am I accumulating belly fat even though I exercise and watch calories?
A: Excess central fat is a signature of altered insulin action. Insulin favors fat storage, especially visceral fat, when tissues become less responsive; that visceral tissue then secretes inflammatory signals that further worsen insulin signaling. Even with calorie control, chronic mild hyperinsulinemia shifts nutrient partitioning toward storage rather than oxidation, so targeted resistance training, protein timing, and carbohydrate quality are often needed to change body composition.
Q: What causes intense sugar or carbohydrate cravings despite being full after meals?
A: Strong cravings usually reflect rapid blood-sugar swings and impaired satiety signaling. If insulin overshoots after a meal, blood glucose can dip below the baseline, triggering hunger and reward-driven eating. Insulin resistance also interacts with leptin and dopamine pathways, making sweet and starchy foods more reinforcing and harder to pass up even when caloric intake is adequate.
Q: Why do my cuts heal slowly and infections linger more than they used to?
A: Insulin supports tissue repair, protein synthesis, and effective immune responses. When insulin signaling falters, cell repair processes, collagen production, and immune cell function are compromised. Microvascular dysfunction and glycation of proteins further reduce local oxygen and nutrient delivery, slowing wound closure and increasing susceptibility to recurrent infections.
Q: What explains new or worsening brain fog, poor focus, and memory slips linked to metabolic issues?
A: The brain depends on steady glucose supply and intact insulin signaling for synaptic function and energy metabolism. Insulin resistance can lead to neuronal energy shortages, increased neuroinflammation, and impaired neurotransmitter balance, producing foggy thinking, slowed processing speed, and short-term memory difficulties-symptoms that often improve when glycemic variability is reduced.
Q: Why does exercise feel less effective for improving energy, and why is recovery poor?
A: Impaired metabolic signaling reduces muscle glucose uptake and mitochondrial adaptation to training, limiting performance gains. Insulin-resistant muscle struggles to switch between fuel sources (metabolic inflexibility), so workouts feel harder and recovery is delayed. Incorporating progressive resistance training, high-intensity intervals, adequate protein, and timed carbohydrate intake can restore responsiveness over weeks to months.
Q: What tests identify disrupted insulin/metabolic signaling and what practical steps help correct it?
A: Useful tests: fasting insulin and glucose, HOMA-IR calculation, HbA1c, oral glucose tolerance test, fasting lipid panel, hs-CRP, and waist circumference assessment. Practical steps: reduce refined carbohydrates and processed sugars, prioritize whole-food protein and fiber, schedule resistance training plus interval cardio, adopt time-restricted eating if tolerated, improve sleep and stress management, and discuss pharmacologic options (e.g., metformin, GLP-1 agonists) with a clinician when lifestyle changes are insufficient. Regular monitoring guides adjustments and tracks improvement.