Nervous system responses determine whether healing advances or stalls, and when your brain registers threat it prioritizes survival over repair; you’ll learn how chronic stress, dysregulated vagal tone, unresolved trauma, inflammation, sleep disruption, autonomic imbalance, and persistent hypervigilance block cellular and psychological recovery, plus practical cues to recognize when your body is wired to hold trauma instead of heal.
Key Takeaways:
- Persistent threat signaling (sympathetic dominance) prioritizes survival over repair, stalling physiological healing.
- Chronic stress hormones (cortisol, adrenaline) drive inflammation and suppress immune functions needed for tissue recovery.
- Hypervigilance redirects metabolic and neural resources away from restorative processes, slowing regeneration.
- Freeze and dissociation block emotional processing and somatic integration, preventing completion of healing cycles.
- Altered interoception and misinterpreted bodily signals maintain pain and symptom patterns that sabotage recovery.
- Sleep disruption impairs neuroplasticity, hormonal balance, and cellular repair necessary for healing.
- Avoidance, mistrust, and reduced engagement with care prevent therapies from producing sustainable change.
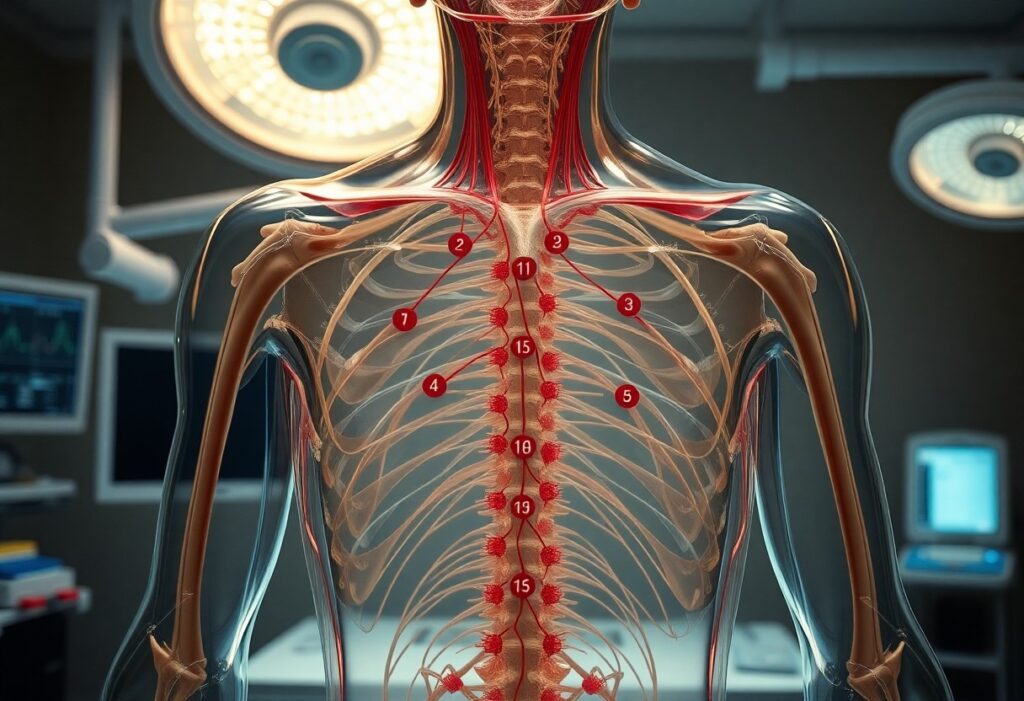
Understanding the Nervous System
You already see how threat signaling hijacks repair; anatomically, the nervous system that does this is split between central processors (prefrontal cortex, amygdala, brainstem) and peripheral effectors. The autonomic branches-the sympathetic and parasympathetic-mediate immediate bodily priorities, with the vagus nerve alone carrying roughly 80% afferent traffic that reports visceral state back to your brain, so shifts in those signals rapidly reconfigure whether your body focuses on rebuilding or just surviving.
The Role of the Autonomic Nervous System
When your sympathetic system activates, blood flow and glucose are redirected to muscles and cognition at the expense of digestion, immunity, and tissue repair; parasympathetic activation restores digestion, lowers heart rate, and supports anabolic processes. You can track this balance via heart rate variability (HRV)-low HRV signals sympathetic dominance-and interventions like HRV biofeedback or vagal stimulation reliably shift physiology toward repair in clinical trials and rehabilitation settings.
Stress Response and its Impact on Health
Acute stress triggers catecholamine release within seconds and activates the HPA axis so cortisol peaks around 20-30 minutes, which is adaptive short-term but harmful if sustained. Chronic elevation of cortisol and norepinephrine suppresses lymphocyte function, alters cytokine profiles (elevated IL‑6/CRP), and reallocates energy away from healing, increasing risk for infections, poor wound closure, hypertension, and metabolic dysregulation over months to years.
Mechanistically, repeated sympathetic surges change immune cell trafficking-neutrophils and monocytes rise while T‑cell proliferation falls-so you see higher baseline inflammation yet poorer targeted immune responses. In real-world terms, caregiving and chronic work stress cohorts demonstrate measurable delays in wound healing and slower vaccine antibody responses, showing how persistent unsafe signaling converts short-term survival chemistry into long-term health deficits.
The Connection Between Safety and Healing
Safety signals recalibrate your body’s priorities: when you sense safety, parasympathetic activity rises, enabling growth-promoting processes like collagen synthesis and tissue perfusion; when threat dominates, cortisol and catecholamines can spike 2-5× and divert resources away from repair. Clinical and experimental work, including caregiver-stress studies, shows chronic threat signaling can slow wound closure by substantial margins and increase infection risk, so the felt environment directly shapes measurable healing trajectories.
Psychological Safety and Physical Recovery
When you experience psychological safety-trust in caregivers, a calming environment, predictable routines-immune and endocrine responses shift toward repair. For example, experimental wound-healing studies found participants with higher perceived social support and lower anxiety healed faster than stressed controls, while patients reporting strong clinician rapport often show reduced postoperative pain and shorter recovery windows. Your subjective sense of safety therefore translates into quantifiable improvements in recovery metrics.
How Threat Perception Alters Healing Processes
Perceiving threat triggers sympathetic vasoconstriction, reduced tissue perfusion, heightened platelet activation and immunosuppression via glucocorticoid signaling, which together impair fibroblast activity and collagen deposition. Acute stress commonly raises heart rate by 20-30 bpm and elevates cortisol, and chronic elevation dampens cytokine cascades needed for the inflammatory-to-repair transition, producing slower wound closure and increased scarring potential.
Threat-driven behaviors compound physiology: you sleep worse, eat poorly, and may skip meds, each independently delaying repair. Neurovisceral markers like low HRV correlate with poorer healing, while interventions that lower threat-vagal stimulation, guided imagery, consistent social support-improve HRV and have been linked in trials to faster tissue repair and reduced inflammatory markers.
The Influence of Trauma on Healing
When trauma remains active in your nervous system, healing loses priority: people with 4+ adverse childhood experiences show roughly 2-4× higher lifetime risk for heart disease, cancer and lung disease, and chronic threat signaling suppresses immune responses. Research on stressed caregivers reports wound-healing delays of about 24-40%, illustrating how persistent sympathetic dominance reduces parasympathetic repair processes and leaves infections, inflammation and tissue regeneration stalled.
Chronic Stress and its Effects on the Body
Chronic stress keeps your HPA axis elevated, driving sustained cortisol release and shifting cytokines toward higher IL-6 and CRP levels-studies report 20-60% increases in inflammatory markers with prolonged stress. That biochemical profile impairs fibroblast activity, decreases collagen synthesis and weakens tensile strength, which translates into slower wound closure and higher infection or complication rates after surgery when stress is unaddressed.
Trauma-Related Disorders and Healing Interruption
PTSD, complex PTSD and persistent dissociation lock your system into hyperarousal and hypervigilance; population estimates put PTSD prevalence around 6-8%, much higher in combat or assault-exposed groups. This sustained sympathetic state disrupts sleep and immune regulation, and some cohort studies show up to a twofold increase in poor post‑operative outcomes, meaning your surgical recovery, chronic wounds or inflammatory conditions are more likely to stall.
Mechanisms compounding these effects include increased norepinephrine from hyperarousal, avoidance-driven delays in seeking care, and comorbidities like substance use, depression and sleep disruption that further blunt repair. You may also face medication-related risks-long-term opioid or benzodiazepine use and untreated insomnia correlate with poorer healing-so trauma-informed assessment, sleep restoration and coordinated pain management often shift trajectories toward improved tissue recovery.
The Role of Mind-Body Connection
When your mental state shifts toward safety, parasympathetic activity increases and repair processes regain priority; chronic anxiety, however, sustains sympathetic arousal, lowers vagal tone, and raises cortisol and IL-6. For example, paced breathing at ~6 breaths per minute reliably boosts HRV and vagal modulation, which correlates with improved tissue repair in experimental studies. You directly influence inflammation and autonomic balance through attention, expectation, and somatic regulation.
The Impact of Mental States on Physical Healing
Negative mental states-persistent worry, rumination, or hopelessness-keep you in a threat-response mode that slows recovery. Caregiver stress models demonstrate delayed biopsy wound closure and elevated inflammatory markers compared with controls. Physiologically, stress episodes can raise heart rate by 10-30 bpm and blood pressure by ~10-20 mmHg, redirecting energy away from cellular repair. You change healing trajectories by modulating cognition and affective responses.
Techniques to Enhance Mind-Body Awareness
You can cultivate interoception and safety signaling with specific, evidence-based practices: resonance breathing (~6 breaths/min) for 10-20 minutes increases HRV, HRV biofeedback across 10-15 sessions enhances vagal tone, progressive muscle relaxation for 10-20 minutes daily reduces somatic tension, and an 8-week body-scan or MBSR protocol improves interoceptive accuracy. Add gentle yoga or guided imagery to anchor sensations to regulatory strategies.
Try a compact daily routine: 2 minutes sensory grounding, 5 minutes resonance breathing at ~6 breaths/min, then a 3-minute body-scan noting tightness and breath. Repeat twice daily for 6 weeks; clinical trials commonly show HRV improvements and reduced perceived stress within 4-8 weeks, while biofeedback protocols (10-15 sessions) yield stronger autonomic gains. Tailor intensity to your baseline tolerance and context for sustainable progress.
Creating a Safe Healing Environment
You can shape safety through predictable routines, clear boundaries, and sensory adjustments: dim lights, reduce background noise below 40-50 dB, and ensure comfortable temperature and seating to lower sympathetic arousal. Use short, timed sessions (30-50 minutes) so expectations are explicit, and introduce paced breathing (4-6 breaths per minute) or brief vagal-stimulating movement before interventions to shift physiology toward repair.
Strategies for Enhancing Emotional Safety
You should practice naming sensations and limits out loud, invite consent before touch or intrusive questions, and use reflective listening to validate experience. Offer grounding tools (5-10% body-weight blankets, textured objects, or weighted lap pads), teach a 4-6 breath paced-breathing drill, and schedule predictable check-ins-these concrete steps reduce uncertainty and improve heart-rate variability linked to better wound and inflammatory outcomes.
The Importance of Support Systems in Recovery
You benefit when social ties provide practical help, emotional containment, and accountability: arrange 2-3 weekly check-ins with a trusted person, join a weekly or biweekly peer support group of 6-12 members, and keep one clinician available for crisis contact. These supports lower perceived threat, promote adherence to care plans, and often reduce medication needs and clinic readmissions.
Different supports serve distinct roles: instrumental help (rides, meals), emotional presence (listening, co-regulation), and informational aid (treatment navigation). You should map who provides each, set boundaries to prevent burnout, and formalize backup plans for setbacks. Consider combining sources-family for logistics, peers for lived-experience insight, and a therapist for clinical containment-to create layered safety that sustains physiological repair over weeks and months.
Conclusion
As a reminder, when your nervous system perceives threat, healing stalls because energy shifts to survival, inflammation persists, sleep and digestion disrupt, and learning and trust are impaired; by addressing safety through regulated breath, movement, predictable routines, and supportive relationships you restore regulation and create the conditions your body needs to complete repair and regain resilience.
FAQ
Q: How does chronic sympathetic activation stop physiological healing?
A: Chronic sympathetic (fight-or-flight) activation raises cortisol and catecholamines, which suppress some immune functions, skew inflammatory responses, constrict blood vessels and reduce tissue perfusion. These hormonal and vascular changes impair cell proliferation, collagen synthesis and angiogenesis needed for wound repair and recovery, so injuries and inflammatory conditions persist or worsen.
Q: Why does persistent hypervigilance make behavioral and biological healing stall?
A: Hypervigilance keeps the nervous system in a state of anticipatory threat, fragmenting sleep and lowering restorative deep and REM sleep stages when growth hormone and many repair processes occur. The result is impaired metabolic recovery, elevated pro-inflammatory cytokines and reduced energy for adaptive immune responses, which slows physical and psychological healing.
Q: In what way do autonomic imbalances – especially low vagal tone – block recovery?
A: Low vagal (parasympathetic) tone weakens the vagus nerve’s anti-inflammatory reflex and reduces heart rate variability, both markers of poor regulatory capacity. Without sufficient parasympathetic engagement the body struggles to downregulate stress-driven inflammation, impairing resolution of injury and prolonging pain and illness.
Q: How do trauma and conditioned threat responses keep the body locked out of healing?
A: Traumatic memories and conditioned cues trigger amygdala-driven defensive cascades that repeatedly activate stress physiology even when no physical danger exists. That repeated activation reinforces neural pathways that maintain sympathetic dominance, perpetuating inflammatory, endocrine and autonomic patterns that interfere with tissue repair and emotional processing.
Q: How does a socially unsafe environment impede the nervous system’s ability to support healing?
A: Perceived social threat-conflict, isolation, unpredictability-elevates stress hormones and lowers oxytocin-mediated safety signaling, making co-regulation and restful states harder to access. Socially unsafe contexts reduce adherence to care, increase inflammation and magnify pain perception, all of which slow recovery.
Q: How do common coping behaviors prevent the nervous system from shifting into healing states?
A: Avoidance, substance use, overexertion, poor sleep and inconsistent medication adherence maintain defensive physiology and delay adaptive processing. These behaviors either perpetuate stress responses (e.g., alcohol disrupting sleep architecture) or deprive the body of nutrients, sleep and rest needed for cellular repair and immune competence.
Q: What practical steps reset safety signals so the nervous system can resume healing?
A: Combine bottom-up regulation (slow diaphragmatic breathing, paced exhalation, HRV biofeedback, grounding and gentle movement) with predictability and social co-regulation (supportive relationships, consistent routines). Add trauma-informed therapies that titrate exposure and build interoceptive tolerance, optimize sleep and nutrition, and coordinate medical care-these strategies shift autonomic balance, reduce inflammation and restore conditions that allow healing to proceed.