Stress rewires your body’s repair systems, shifting hormones like cortisol and adrenaline into patterns that silently impede healing and cellular regeneration. Over time these hormonal shifts suppress immune responses, disrupt sleep-driven restoration, impair mitochondrial function, increase inflammation, alter blood flow to tissues, weaken connective tissue synthesis, and interfere with DNA repair pathways, so your recovery becomes slower and more error-prone. Understanding these mechanisms helps you target interventions that restore resilience and repair.
Key Takeaways:
- Chronic cortisol and catecholamines suppress immune cell function and cytokine signaling, delaying wound closure and infection control.
- Prolonged stress causes immune dysregulation-persistent, low-grade inflammation with impaired resolution-slowing tissue repair.
- High glucocorticoids inhibit collagen synthesis and fibroblast activity, reducing extracellular matrix formation and structural healing.
- Stress-driven insulin resistance and hyperglycemia impair cellular nutrient uptake and promote protein glycation that weakens repair processes.
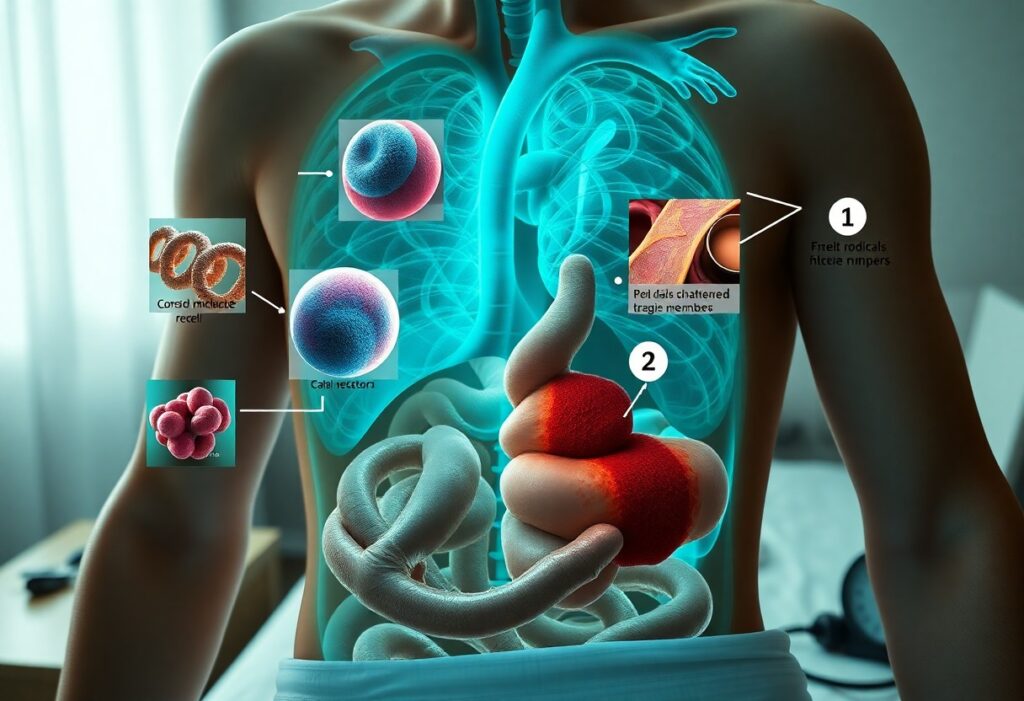
- Stress hormones damage mitochondria and increase reactive oxygen species, lowering ATP availability and amplifying DNA and cellular damage.
- Sustained cortisol suppresses growth hormone and sex steroids and impairs stem/progenitor cell function, reducing cell proliferation and regeneration.
- Chronic sympathetic activation and circadian disruption constrict blood flow, limit oxygen/nutrient delivery, and interfere with sleep-dependent repair mechanisms.
Understanding Stress Hormones
When stress becomes chronic, your endocrine signals shift from brief alarms to sustained hormonal patterns that reprogram repair. These persistent elevations change immune-cell trafficking, dampen growth-factor signaling, and reduce collagen synthesis, so wounds and tissues take longer to rebuild and cellular housekeeping (autophagy, DNA repair) becomes less efficient.
The Role of Cortisol
Cortisol from your adrenal cortex normally peaks 30-45 minutes after waking (the cortisol awakening response) and ranges roughly 5-25 µg/dL in the morning. When chronically elevated it mobilizes glucose but suppresses lymphocyte function, reduces fibroblast-driven collagen production, and downregulates growth factors-mechanisms shown in caregiver studies to produce significantly slower wound healing and impaired vaccine responses.
Other Key Hormones in Stress Response
Epinephrine and norepinephrine spike within seconds, raising heart rate and redistributing leukocytes; DHEA opposes some cortisol effects but declines with age; insulin and growth hormone shifts under stress alter nutrient supply for repair; and suppressed sex hormones (testosterone, estrogen) reduce tissue regeneration-together these shifts promote low-grade inflammation (IL-6, TNF-α) that impedes cellular recovery.
Adrenergic signaling acts directly on immune cells via α/β receptors, so when your norepinephrine stays high NF-κB-driven IL-6 and TNF-α increase and leukocyte trafficking shifts away from repair. A low DHEA:cortisol ratio predicts poorer immune resilience, while stress-induced hyperglycemia and insulin resistance promote protein glycation that weakens collagen cross-links-factors linked in clinical cohorts to higher postoperative infection rates and delayed graft or wound integration.
Chronic Stress and Its Impact on Healing
When stress becomes sustained, your body reallocates resources away from repair: energy, blood flow, and immune attention favor immediate survival over rebuilding. You experience slower wound closure, impaired tissue remodeling, and a higher chance of infection or fibrosis; for example, caregiver cohorts repeatedly show measurable delays in wound healing and altered inflammatory responses, linking everyday psychosocial stressors to tangible deficits in recovery and tissue integrity.
Disruption of Cellular Repair Processes
At the cellular level, prolonged cortisol and catecholamine exposure reduces telomerase activity, accelerates telomere shortening, and impairs DNA repair enzymes, so your cells accumulate damage faster. Fibroblast proliferation and collagen synthesis decline, mitochondrial function falters, and autophagy pathways become dysregulated-together these changes slow tissue regeneration and increase the likelihood of chronic, nonhealing wounds.
Inhibition of Immune Function
Chronic stress suppresses key immune defenses: natural killer cell activity falls, lymphocyte proliferation drops, and antibody responses to antigens become weaker, leaving you more vulnerable to infection. Clinical studies show stressed individuals-students during exams or long-term caregivers-often exhibit reduced vaccine responses and increased incidence of respiratory infections compared with low-stress peers.
Mechanistically, sustained glucocorticoid signaling alters gene transcription in immune cells, downregulating IL‑2 and interferon‑γ, shifting away from effective Th1-mediated clearance toward impaired cellular immunity. Catecholamines disrupt neutrophil and macrophage trafficking and reduce antigen presentation, while persistent inflammation paradoxically coexists with immune suppression. In some caregiver and chronically stressed cohorts, NK cytotoxicity and specific antibody titers can be reduced by roughly 30-50% or more, translating into slower bacterial clearance, higher infection rates, and delayed wound healing in real-world patient samples.
Emotional and Psychological Effects of Chronic Stress
Emotional strain from ongoing stress rewires your mood and coping: you become more reactive, less motivated, and slower to seek care, which undermines recovery. Research links sustained stress exposure with about a twofold increase in depressive episodes and chronic anxiety, and many patients report persistent sleep disruption that further impairs immune and tissue repair.
Mental Health Correlations
Chronic elevations of cortisol and catecholamines correlate with clinically measurable changes: MRI studies show hippocampal volume reductions of roughly 5-10% in stress-related disorders and increased amygdala reactivity that heightens threat perception. As a result, you face higher rates of major depressive disorder, generalized anxiety, and PTSD-like symptoms, each of which interferes with adherence to medical regimens and rehabilitation.
Influence on Lifestyle and Self-Care
Under prolonged stress you’re likelier to skip sleep, exercise, and basic wound care; behavioral data indicate physically active time can drop by around 30% and unhealthy eating rises substantially. Those shifts compound hormonal disturbances-less sleep reduces nocturnal growth hormone pulses-so your habits directly slow cellular repair and increase infection risk.
Practically, stress impairs executive function in the prefrontal cortex, making short-term comfort choices (junk food, alcohol, missed appointments) more appealing despite long-term harm; workplace studies of 1,200 adults show high perceived stress doubles the likelihood of inactivity and increases reports of medication nonadherence. Addressing these behaviors-structured sleep schedules, brief daily walks, and simplified adherence strategies-restores repair processes and improves healing trajectories.
Physiological Changes Linked to Chronic Stress
Your body shifts into a conservation mode where blood flow, cellular energy, and repair pathways are deprioritized: mitochondrial ATP production falls, oxidative damage rises, and immune surveillance weakens. Studies of long-term caregivers link chronic psychosocial stress with accelerated telomere shortening equivalent to roughly 9-17 years of cellular aging, while sustained sympathetic drive increases resting heart rate and blood pressure, diverting resources from tissue repair and raising your risk for delayed wound healing and chronic disease.
Effects on Inflammation
Initially anti-inflammatory cortisol gives way to glucocorticoid receptor resistance under chronic exposure, so you end up with higher circulating IL-6 and C-reactive protein; meta-analyses report roughly a 20-30% elevation in CRP among chronically stressed groups. For example, dementia caregivers and people with PTSD consistently show elevated pro-inflammatory cytokines and slower resolution of inflammation after injury, which directly impairs tissue remodeling and infection defense.
Impact on Hormonal Balance
Chronic stress dysregulates the HPA axis, producing a flattened diurnal cortisol rhythm-morning peaks can be blunted by ~15-25% while evening levels stay abnormally high-disrupting sleep and downstream hormones. You’ll often see reduced DHEA and sex steroids (lower testosterone in men, altered estrogen/progesterone cycles in women), plus impaired thyroid signaling, all of which undermine anabolic repair processes and metabolic homeostasis.
More specifically, prolonged cortisol excess suppresses gonadotropin-releasing hormone and thyroid-stimulating hormone, so you may experience irregular menses, reduced fertility, diminished libido, and lower bone formation; epidemiological data link chronic stress to about a 1.4-1.6-fold increased odds of metabolic syndrome, driven by visceral fat gain, insulin resistance, and the hormonal milieu that blunts cellular regeneration.
Strategies for Mitigating Stress
Try a multi-pronged plan that combines short daily practices with lifestyle shifts: 10-20 minutes of targeted breathing or meditation, 30-60 minutes of moderate exercise most days, sleep scheduling of 7-9 hours, and dietary tweaks like two fatty fish servings weekly. Together these lower sympathetic tone, support parasympathetic recovery and free up metabolic resources for cellular repair, so you get measurable reduction in stress burden over weeks rather than months.
Mindfulness and Relaxation Techniques
Start with 5-10 minutes of diaphragmatic breathing (≈6 breaths/min) or box breathing (4‑4‑4‑4) to boost your HRV; you can add a 10-20 minute body‑scan or guided meditation three times weekly. Incorporate progressive muscle relaxation in the evening to reduce your nighttime arousal, and use HRV biofeedback or smartphone apps to track your progress-consistency of 10-20 minutes daily typically yields physiological shifts within 2-8 weeks.
Nutritional and Lifestyle Approaches
Prioritize a Mediterranean-style pattern-vegetables, fiber, olive oil, nuts-and two servings of fatty fish per week for omega‑3s; reduce added sugars and refined carbs to avoid glycemic spikes that amplify your cortisol. Keep to 7-9 hours sleep with fixed sleep/wake times, and aim for 150 minutes moderate aerobic activity plus two strength sessions weekly to lower inflammation and promote mitochondrial resilience.
Focus on micronutrients and routines that support your repair: check your vitamin D status and prioritize magnesium-rich foods (leafy greens, nuts, legumes) plus fermented foods for gut-brain signaling. Consider a 10-12 hour overnight eating window to improve metabolic flexibility, and track your results with sleep metrics, resting HRV, and basic labs (CRP, fasting glucose) every 3-6 months to quantify improvements linked to your changes.
Summing up
Taking this into account, chronic activation of stress hormones undermines your healing and cellular repair by promoting inflammation, impairing immune responses, disrupting sleep and hormone balance, increasing oxidative damage, reducing tissue regeneration, and altering metabolic resources; by recognizing these pathways you can prioritize interventions that lower stress hormone exposure and restore the physiological conditions needed for effective repair.
FAQ
Q: How does prolonged cortisol exposure impair tissue repair?
A: Chronic elevation of cortisol drives catabolism that inhibits fibroblast proliferation, reduces collagen synthesis and angiogenesis, and suppresses local growth factors. Those effects slow wound closure, weaken repaired tissue, and delay remodeling after injury.
Q: How do sustained catecholamines and sympathetic overdrive block healing?
A: Persistent norepinephrine and epinephrine cause vasoconstriction and reduced microcirculatory perfusion, limiting oxygen and nutrient delivery to damaged tissue. They also alter leukocyte trafficking and increase platelet aggregation, which impairs clearance of debris and formation of healthy granulation tissue.
Q: In what ways does chronic stress dysregulate immune function and inflammation?
A: Long-term stress shifts immune balance toward persistent, low-grade inflammation while impairing coordinated innate and adaptive responses. That means slower pathogen clearance, excessive pro-inflammatory cytokine signaling, disrupted macrophage transition from inflammatory to repair phenotypes, and poorer tissue remodeling.
Q: How does chronic stress accelerate cellular aging and telomere shortening?
A: Elevated stress hormones and associated oxidative damage increase telomere attrition and DNA damage, promoting cellular senescence. Senescent cells secrete pro-inflammatory factors (SASP) and reduce stem/progenitor cell renewal, undermining regeneration and repair capacity.
Q: Why does disrupted sleep and circadian rhythm interfere with cellular repair?
A: Sleep loss and circadian disruption blunt nocturnal release of growth hormone and melatonin, impair DNA repair enzyme activity, and disturb timed immune functions. The result is reduced tissue synthesis, impaired removal of metabolic waste, and slower recovery processes.
Q: How do stress-driven mitochondrial dysfunction and oxidative stress hinder healing?
A: Chronic stress increases reactive oxygen species and damages mitochondrial DNA and membranes, lowering ATP production needed for energy-intensive repair processes. Energy shortfalls, increased apoptosis, and more oxidative injury together impede effective cellular restoration.
Q: Can stress produce lasting gene-level changes that block repair?
A: Yes. Repeated stress can induce epigenetic modifications-DNA methylation and histone changes-that downregulate genes for growth factors, antioxidant enzymes, and repair pathways. Those persistent changes make tissues less responsive to regenerative signals and slow long-term healing.