Many of your cells rely on autophagy to recycle damaged proteins and organelles, improving cellular energy efficiency, supporting tissue repair, reducing inflammation, enhancing metabolic health, protecting against neurodegeneration, promoting immune function, and extending healthy lifespan; understanding how to safely stimulate autophagy through nutrition, fasting patterns, exercise, and sleep empowers you to optimize recovery, resilience, and long-term vitality.
Key Takeaways:
- Removes damaged proteins and organelles to prevent cellular buildup and dysfunction.
- Recycles cellular components into fuel, improving energy availability during fasting or stress.
- Maintains mitochondrial health (mitophagy), enhancing ATP production and metabolic efficiency.
- Supports tissue repair and maintenance, associated with delayed age-related decline and increased lifespan in models.
- Reduces protein aggregates and supports immune responses, lowering risk of neurodegenerative and other diseases.
- Lowers inflammation and oxidative stress by clearing inflammasome activators and damaged molecules.
- Activated by fasting, calorie restriction, exercise, and certain compounds (mTOR inhibition/AMPK activation); activity declines with age.
Understanding Autophagy
When you want to optimize cellular cleanup, autophagy recycles damaged proteins and organelles to free amino acids and lipids for energy and repair. Nutrient-sensing kinases such as mTOR and AMPK rapidly shift autophagy rates; rodent models show strong induction after 16-48 hours of fasting, and small human studies report increased LC3-II after ~24 hours, while intense exercise and caloric restriction also produce measurable upregulation.
Definition and Mechanism
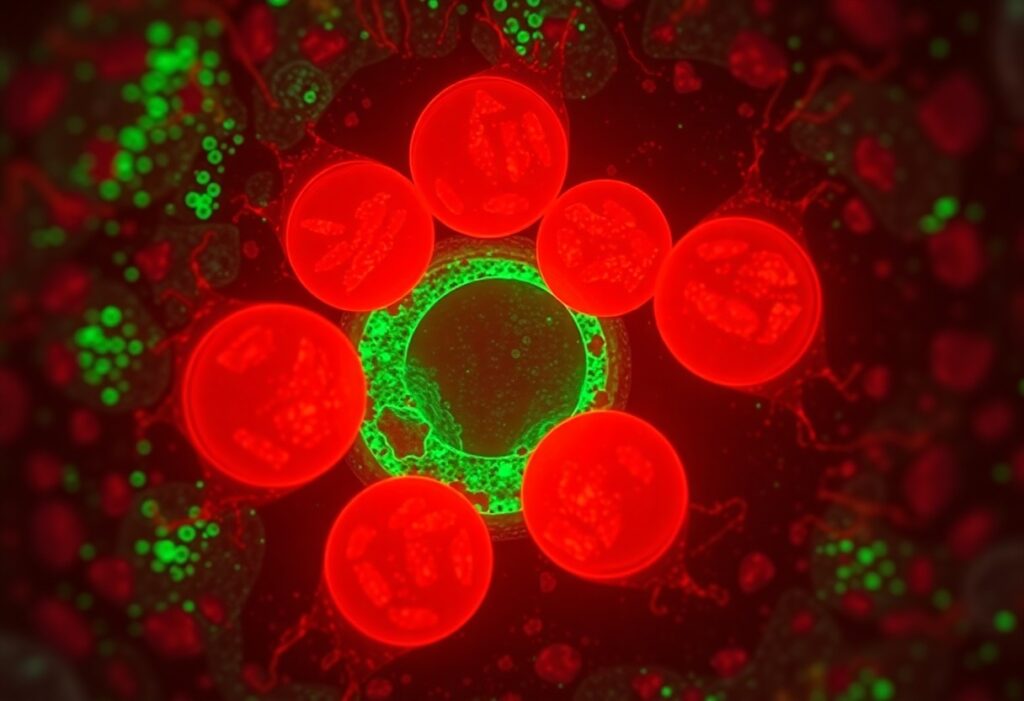
Macroautophagy, the primary pathway, starts when mTOR inhibition or AMPK activation engages the ULK1 complex to nucleate a phagophore; Atg proteins and LC3 lipidation then elongate the membrane into an autophagosome, which fuses with lysosomes for degradation. Yeast genetics uncovered ~30 core ATG genes, many conserved in mammals, so you can follow distinct steps from initiation (ULK1) through LC3-II tagging to lysosomal hydrolase-mediated recycling.
Historical Perspective
Christian de Duve coined “autophagy” in 1963 after electron-microscopy studies of lysosomes and later received the 1974 Nobel for that work. You should note the field’s pivotal shift in the 1990s when Yoshinori Ohsumi used yeast genetics to identify ATG genes, a breakthrough that culminated in his 2016 Nobel and transformed autophagy into a defined molecular pathway with therapeutic promise.
Early electron-microscopy observations in the 1950s set the descriptive stage, but Ohsumi’s 1993 experiments-blocking vacuolar proteases to reveal accumulating autophagic bodies and isolating mutants-mapped the first core ATG genes. From there, systematic screens expanded the list (roughly 30 core genes in yeast with mammalian homologs), enabling biochemical dissection of ULK1, Beclin-1, ATG7 and LC3 conjugation systems. Today, when you scan translational work you’ll find mTOR inhibitors like rapamycin used to induce autophagy, lysosomal inhibitors such as chloroquine employed to block it in oncology trials, and lifespan studies in C. elegans and mice linking intact autophagy genes to longevity-evidence that historical genetics directly shaped current clinical strategies.
The Role of Autophagy in Energy Production
Metabolic Efficiency
Autophagy recycles damaged proteins and organelles into amino acids and fatty acids that feed gluconeogenesis and beta‑oxidation, helping your cells sustain ATP production during nutrient scarcity. Time‑restricted feeding (for example, a 16:8 pattern) and 24‑hour fasts have been shown to raise autophagy markers and improve insulin sensitivity, so your metabolism becomes more flexible and switches between glucose and fat oxidation with greater efficiency.
Mitochondrial Health
Mitophagy removes dysfunctional mitochondria to reduce reactive oxygen species and preserve ATP output, which supports your endurance and cellular repair. The PINK1-Parkin pathway flags depolarized mitochondria for clearance, and Parkin mutations are linked to early‑onset Parkinson’s, showing how impaired mitophagy damages neurons. Enhanced mitophagy in animal models associates with better mitochondrial function and delayed age‑related decline.
At the molecular level, PINK1 accumulates on mitochondria that lose membrane potential, recruiting Parkin to ubiquitinate outer‑membrane proteins and trigger autophagosome engulfment; BNIP3/NIX act as receptor‑mediated pathways under hypoxia. You can track mitophagy by increased LC3‑II and decreased p62 co‑localizing with mitochondrial markers. In rodents, single exercise sessions (30-60 minutes) and 16-24 hour fasts elevate mitophagy markers and improve mitochondrial respiration and muscle performance.
Cellular Repair and Maintenance
By targeting damaged components for degradation, autophagy lets you maintain cellular integrity and slows accumulation of senescent material; fasting and exercise can raise autophagic flux several-fold, reflected by increased LC3-II and reduced p62 in tissues. This turnover supplies amino acids for repair, limits oxidative stress, and supports tissue resilience-for example, enhanced autophagy in mouse models preserves muscle function after prolonged nutrient stress.
Protein Homeostasis
You rely on multiple autophagy pathways to maintain protein balance: chaperone-mediated autophagy (CMA) recognizes KFERQ-like motifs for direct lysosomal import, while macroautophagy engulfs large aggregates such as mutant huntingtin or α-synuclein. When these pathways are boosted experimentally, aggregate load falls and cell viability improves in neurodegeneration models, demonstrating how autophagy preserves proteome quality.
Removal of Damaged Organelles
Mitophagy, pexophagy and ER-phagy selectively eliminate dysfunctional organelles so your cells retain metabolic efficiency and limit harmful ROS production; mitophagy targets mitochondria with low membrane potential, preventing ATP leakage and oxidative damage, while pexophagy removes oxidized peroxisomes that would otherwise amplify lipid peroxidation.
At the molecular level, depolarized mitochondria accumulate PINK1 on the outer membrane, which recruits Parkin to ubiquitinate outer membrane proteins and mark them for autophagosome engulfment; receptor proteins like NIX/BNIP3 or mitophagy adaptors (e.g., OPTN, NDP52) then bind LC3 to complete removal. Impairments in this cascade (PINK1/Parkin defects) are linked to neurodegenerative phenotypes in animal and human studies, highlighting the pathway’s physiological importance.
Autophagy and Longevity
Impact on Aging Processes
When autophagy falters with age, you accumulate damaged proteins, dysfunctional mitochondria, and senescent cells that accelerate tissue decline. Experimental activation of autophagy extends lifespan in yeast, C. elegans, and Drosophila and improves healthspan metrics in mice. Mechanistically, you benefit from enhanced proteostasis, mitochondrial turnover, and reduced inflammation-changes that collectively slow functional decline and lower the incidence of age-related pathologies.
Caloric Restriction and Autophagy
Caloric restriction (commonly 20-40% in rodent studies) and fasting activate autophagy by inhibiting mTOR and activating AMPK and sirtuins; you can begin to detect autophagic flux after ~12-24 hours of fasting, with stronger induction at 24-48 hours. In many models, the longevity gains from caloric restriction require intact autophagy genes, linking your dietary approach directly to cellular cleanup mechanisms.
Time-restricted feeding (e.g., 16:8) often improves metabolic markers but typically induces milder autophagy than multi-day fasting or strict CR; you’ll see stronger autophagic responses when combining fasting with exercise, which activates AMPK in muscle. Nutrient composition also matters-protein or branched-chain amino acids blunt autophagy via mTOR-so strategic fasting windows or periodic 24-48 hour fasts tend to produce the most consistent autophagy-related benefits in humans and animal models.
Autophagy in Disease Prevention
By maintaining proteostasis and mitochondrial quality, autophagy lowers the burden of DNA damage, inflammation, and metabolic stress that drive many diseases. Beclin‑1 haploinsufficiency increases tumor formation in mouse models, illustrating how genetic defects in autophagy raise disease risk. You can modulate autophagy through intermittent fasting, exercise, or mTOR inhibition-approaches that reduce pathology in models of metabolic disease, infection, and degeneration.
Cancer and Autophagy
Your autophagy suppresses tumor initiation by clearing damaged mitochondria and misfolded proteins, limiting ROS and genomic instability. However, established cancers exploit autophagy to survive hypoxia and chemotherapy; pancreatic ductal adenocarcinoma shows pronounced autophagy dependence. Trials have combined hydroxychloroquine with chemotherapy to block autophagy, and Beclin‑1 loss in human tumors mirrors pro‑tumor effects observed in mice.
Neurodegenerative Disorders
Efficient autophagy prevents accumulation of aggregation‑prone proteins-amyloid‑beta, tau, and alpha‑synuclein-that drive Alzheimer’s and Parkinson’s. In your neurons, deficits in autophagosome formation or lysosomal clearance have been documented in patient brains and mouse models. Enhancing autophagy with rapamycin, TFEB activation, or clearance enhancers reduces aggregates and improves cognition or motor function in multiple preclinical studies.
Mechanistically, your neurons often show stalled autophagic flux: autophagosomes accumulate in dystrophic neurites due to lysosomal dysfunction. Genetic factors such as GBA and LRRK2 impair lysosomal-autophagy pathways and increase Parkinson’s risk, while declines in Beclin‑1 or ATG genes correlate with Alzheimer’s pathology. Strategies like ambroxol for GBA carriers, lysosomal acidification boosters, and TFEB agonists are progressing in clinical development to restore clearance and slow degeneration.
Stimulating Autophagy Naturally
You can amplify cellular cleanup through a mix of diet, movement, sleep, and targeted nutrients; evidence shows combined interventions produce stronger autophagy signals than any single change. In animal studies, 20-30% caloric restriction extends lifespan by ~20-40% and intermittent fasting protocols (16:8 or 24-48-hour fasts) reliably upregulate autophagy markers. Practical adjustments-timed feeding, protein distribution, and polyphenol-rich foods-help you shift metabolism toward efficient recycling without relying on drugs.
Dietary Interventions
Time-restricted eating (eg, 16:8) and periodic 24-48 hour fasts are among the most reproducible ways you trigger autophagy; they lower insulin and mTOR signaling while raising AMPK. You should also moderate total protein and leucine intake around the clock to avoid constant mTOR activation, and incorporate spermidine sources (wheat germ, aged cheese, mushrooms) plus polyphenols like EGCG and resveratrol to support autophagic pathways.
Exercise and Lifestyle Factors
Regular aerobic and resistance training activate AMPK and mitophagy: aim for 30-60 minutes of moderate exercise 3-5 times weekly or 20-30 minute HIIT sessions to stimulate muscle autophagy. Good sleep (7-9 hours), circadian-aligned meals, and avoiding chronic alcohol help maintain basal autophagy rhythms, while acute stressors like cold exposure or brief fasting before workouts can further amplify the response.
- Intermittent fasting options: 16:8 daily, alternate-day fasting, or occasional 24-48 hour fasts to robustly induce autophagy.
- Diet composition: lower peri-meal leucine, include spermidine-rich and polyphenol foods, and consider 20-30% caloric reduction when sustainable.
- Recognizing that timing-when you eat, train, and sleep-often matters more than single food choices for consistent autophagy activation.
For exercise specifically, you should prioritize consistency and progressive overload: a single 30-45 minute aerobic session raises autophagy markers in human muscle within hours, while adding resistance training twice weekly enhances proteostasis and mitochondrial turnover. Combining fasted-state low-moderate cardio with post-workout protein timed to your goals balances autophagic benefit and recovery; athletes often cycle intensity to avoid chronic catabolism while preserving cellular cleanup.
- Practical tips: train fasted occasionally, avoid late-night high-calorie meals, and aim for 7-9 hours of sleep to align autophagy with circadian biology.
- Recovery matters: keep alcohol low and manage chronic stress to prevent autophagy suppression from prolonged inflammation.
- Recognizing that individualized protocols-based on age, activity level, and medical history-yield the best long-term balance between repair and performance.
Final Words
Upon reflecting, you can see how autophagy optimizes cellular cleanup to boost your energy, accelerate repair, reduce cellular damage, support metabolic balance, and promote longevity; by integrating targeted fasting, exercise, and nutrient strategies you enhance cellular renewal and resilience, giving your body a measurable foundation for improved health span and sustained vitality.
FAQ
Q: What is autophagy and how does it function as cellular cleanup?
A: Autophagy is a regulated process cells use to degrade and recycle damaged proteins, organelles, and other intracellular debris. Cells form double-membrane vesicles called autophagosomes around targeted material, then fuse them with lysosomes where enzymes break contents down into basic building blocks (amino acids, fatty acids, sugars) that the cell reuses for energy and biosynthesis. Autophagy operates constitutively at baseline and is upregulated in response to stressors such as nutrient scarcity, oxidative stress, and exercise.
Q: How does autophagy improve cellular energy availability?
A: By breaking down dysfunctional mitochondria and oxidatively damaged components, autophagy frees metabolic substrates and reduces energy-wasting processes. Mitophagy (selective removal of damaged mitochondria) improves mitochondrial quality and efficiency, lowering reactive oxygen species production and increasing ATP output per nutrient unit. During fasting or nutrient restriction, autophagy supplies amino acids and fatty acids that sustain ATP production until external nutrients are available again.
Q: In what ways does autophagy promote cellular repair and protein quality control?
A: Autophagy clears misfolded and aggregated proteins that the proteasome cannot handle, preventing proteotoxic stress and preserving proteome integrity. It also removes damaged organelles (e.g., ER, mitochondria), mitigating dysfunctional signaling and membrane damage. This turnover supports synthesis of new, functional proteins and organelles, enhances stress resilience, and maintains cellular architecture required for normal function.
Q: What evidence links autophagy to increased lifespan and protection against age-related diseases?
A: In multiple model organisms, genetic or pharmacologic enhancement of autophagy extends lifespan and delays age-associated decline. Improved clearance of protein aggregates and damaged organelles lowers risk for neurodegenerative diseases (Alzheimer’s, Parkinson’s), maintains metabolic homeostasis to reduce cardiometabolic disease risk, and supports genomic stability. Human data are associative but consistent with benefits seen in animal studies; balanced autophagy appears to be a conserved mechanism that promotes healthy aging.
Q: Which metabolic and immune benefits does autophagy provide?
A: Autophagy contributes to metabolic flexibility by supporting gluconeogenesis and lipid mobilization during fasting, improving insulin sensitivity, and reducing ectopic lipid accumulation. In immunity, autophagy helps remove intracellular pathogens, presents antigens, and regulates inflammatory signaling by degrading inflammasome components and damaged mitochondria that would otherwise release pro-inflammatory molecules.
Q: What practical strategies reliably stimulate autophagy?
A: Physiologic triggers include intermittent fasting, time-restricted eating, caloric restriction, regular aerobic and resistance exercise, and periods of carbohydrate restriction that induce ketosis. Certain compounds (e.g., spermidine, resveratrol) and drugs (e.g., mTOR inhibitors) can modulate autophagy, but their use should be guided by a clinician. Combining nutritional timing with consistent exercise and adequate sleep yields the most reproducible increases in autophagic activity for most people.
Q: Are there risks or limits to enhancing autophagy, and when should one be cautious?
A: Excessive or prolonged autophagy can contribute to tissue wasting, impaired immune responses, or cell death in vulnerable contexts. In people with active infections, certain cancers, or frailty, stimulating autophagy without medical supervision may be harmful. Pharmacologic autophagy modulators can have off-target effects and drug interactions. Clinical consultation is recommended before pursuing extreme dietary, pharmacologic, or prolonged fasting protocols.