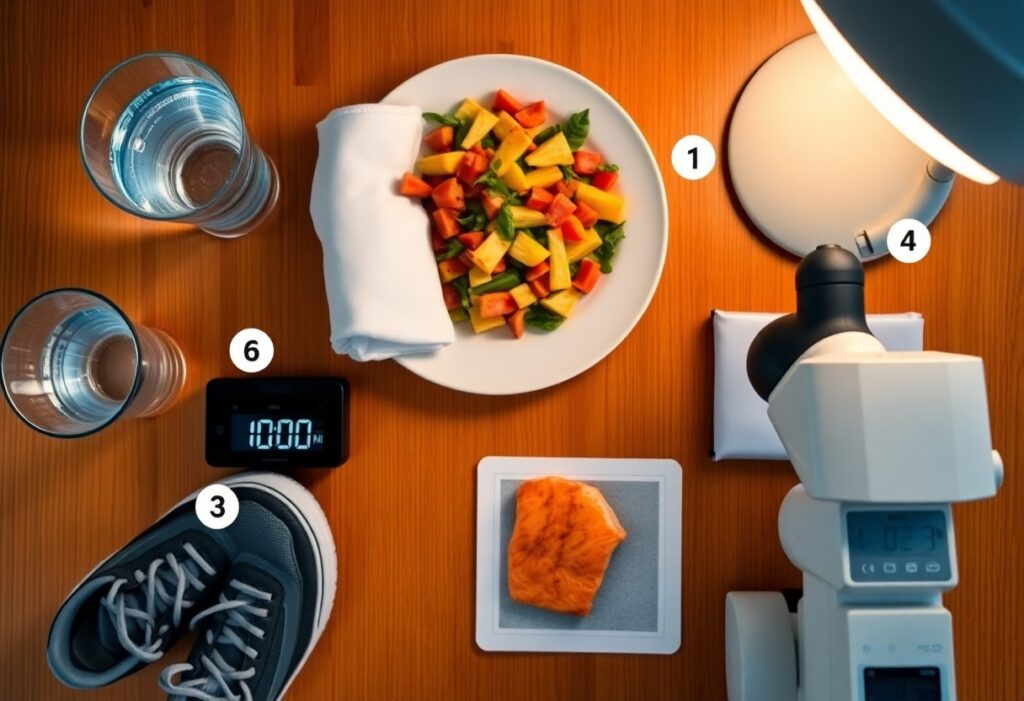
Most people seeking meaningful recovery overlook that deep cellular repair requires five proven conditions you must support: restorative sleep, nutrient-dense intake, effective inflammation regulation, adequate blood flow and oxygenation, and balanced hormonal/metabolic signaling; when you optimize these factors, your body can perform the cellular maintenance and regeneration necessary for lasting healing.
Cellular Repair: Core Biology
Your cells rely on coordinated energy supply, signaling and structural support to move from damage control to deep repair. Mitochondrial ATP, proteostasis, and intact DNA repair pathways (NER, BER, HR, NHEJ) must be operational while immune surveillance clears dysfunctional cells. Failures in any of these-reduced autophagy, impaired repair enzymes, or a hostile microenvironment-shift tissues into chronic dysfunction rather than restoration.
Key mechanisms – autophagy, DNA repair, senescent cell clearance
Autophagy removes damaged organelles and protein aggregates, often rising during 16-48 hour fasts to increase clearance capacity. DNA repair pathways target specific lesions: BER fixes oxidative 8-oxo-dG, NER removes bulky adducts, HR/NHEJ resolve double-strand breaks. Senescent cells emit a pro-inflammatory SASP (IL-6, IL-8) and are normally cleared by NK cells and macrophages; senolytic interventions (dasatinib+quercetin) reduced senescent burden and improved function in mouse studies.
The cellular environment – inflammation, oxidative stress, extracellular matrix
Persistent inflammation (elevated TNF-α, IL-6) and excess reactive oxygen species generate oxidative lesions and lipid peroxides that overwhelm repair systems. Altered extracellular matrix-excess collagen crosslinking, fibronectin fragmentation, or high MMP activity-disrupts stem cell niches and mechanical cues, so even competent cells cannot re-establish organized tissue architecture.
In chronic wounds, for example, MMP-9 levels remain high while TIMP inhibitors stay low, driving proteolytic ECM degradation and stalled healing; diabetic ulcers illustrate this imbalance. You can detect oxidative damage via markers like 8-oxo-dG or malondialdehyde; elevated levels correlate with poorer outcomes. Interventions that lower ROS (N‑acetylcysteine), modulate MMP activity, or restore ECM mechanics have shown measurable improvements in tissue repair in preclinical and clinical pilot studies.
Condition 1 – Nutrition & Cofactors
You need specific macronutrients and micromineral cofactors to drive repair; priority nutrients include:
- Protein 1.2-2.0 g/kg/day; leucine ~2-3 g/meal for muscle and collagen synthesis
- Vitamin C 500-1,000 mg/day for collagen hydroxylation
- Zinc 15-30 mg/day for DNA replication and immune cell proliferation
- Vitamin D 1,000-4,000 IU/day and iron/B12 if deficient
- Omega‑3 EPA/DHA 1-3 g/day to modulate inflammation
Assume that you integrate these into meals and targeted supplements during recovery.
Macronutrients and crucial micronutrients for repair
Aim for protein 1.2-2.0 g/kg/day to support tissue synthesis and immune function, distribute 20-40 g protein per meal, supply 40-60% of calories from carbs to fuel glycolysis and spare protein, and include 20-35% of calories from fats with 1-3 g/day EPA/DHA. Add vitamin C (500-1,000 mg/day), zinc (15-30 mg/day), vitamin D (1,000-4,000 IU/day) and correct iron/B12 deficiencies to optimize collagen formation, ATP generation, and DNA repair.
Practical dietary patterns and supplementation priorities
Follow a protein‑focused, anti‑inflammatory pattern: oily fish twice weekly, colorful vegetables, whole grains, and 1-2 high‑vitamin C fruits daily; use protein‑fortified meals or shakes to hit per‑meal targets. Prioritize a quality multivitamin for gaps, 1-3 g/day fish oil for inflammation, and targeted zinc or vitamin D after testing. You should time protein and carbs around activity to amplify repair signaling.
In clinical or high‑stress recovery, protocols often prescribe ~1.5 g/kg/day protein plus 20-40 g collagen hydrolysate daily with 500-1,000 mg vitamin C to improve wound tensile strength; pair with 25-50 g carbs within two hours post‑exercise for glycogen repletion. For vitamin D deficiency, supervised loading (e.g., 50,000 IU weekly for 6-8 weeks) then 2,000 IU/day maintenance is common, and EPA 1-2 g/day is practical for lowering pro‑inflammatory markers.
Condition 2 – Sleep and Circadian Alignment
Poor alignment between your sleep schedule and circadian rhythm undermines cellular repair; adults need 7-9 hours of consolidated sleep and consistent timing to optimize hormonal pulses and immune recovery. Shift work or irregular schedules elevate inflammatory markers and slow wound healing, so stabilizing sleep onset within a roughly 30-60 minute window each night preserves the timing of repair processes and improves outcomes like tissue regeneration and metabolic resilience.
Sleep-stage processes that enable deep repair (growth hormone, glymphatic clearance)
During deep slow-wave sleep (SWS) your pituitary releases the largest nocturnal growth hormone pulse, typically within the first 60-90 minutes, driving protein synthesis and tissue repair. At the same time glymphatic clearance ramps up-rodent studies show up to a 10-fold increase in interstitial fluid flux during sleep-helping remove misfolded proteins and metabolic waste that would otherwise impair cellular recovery.
Strategies to restore circadian rhythm and sleep quality
Set a fixed wake time, expose yourself to 20-30 minutes of morning light, avoid screens 1-2 hours before bed, keep the bedroom near 65°F (18°C), limit caffeine after 2 p.m., and consider low-dose melatonin (0.5-1 mg) 1-2 hours before sleep to shift timing and improve sleep onset and continuity.
If you’re phase-delayed, use morning bright light (10,000 lux for 20-30 minutes) within 30 minutes of waking and 0.5 mg melatonin an hour before bedtime to advance your clock; night-shift workers benefit from strategic bright light during shifts, blackout curtains for daytime sleep, and a 20-90 minute anchor nap before work. Track sleep with actigraphy or a sleep diary and aim for consistent sleep windows within ±30 minutes to restore SWS depth and glymphatic efficiency.
Condition 3 – Immune Balance and Inflammation Control
Your immune response must shift from rapid clearance to controlled resolution for deep healing to proceed. Excessive M1 macrophage and neutrophil activity raises MMPs (e.g., MMP‑9) that degrade extracellular matrix, while M2 phenotypes support collagen deposition and angiogenesis. Clinically, CRP >3 mg/L signals heightened systemic inflammation and is linked to slower wound closure and fibrotic remodeling; you need timely cytokine downregulation to permit stem-cell driven tissue regeneration.
Distinguishing acute versus chronic inflammation and their effects on repair
Acute inflammation (minutes-48/72 hours) brings neutrophils, edema and growth-factor signals that clear debris and kick-start proliferation; chronic inflammation (weeks-years) features macrophages, lymphocytes and persistent TNF/IL‑6 that sustain protease activity and prevent productive matrix formation. In diabetics, for example, prolonged neutrophil influx and elevated MMPs correlate with non-healing ulcers and impaired angiogenesis, demonstrating how unresolved inflammation converts repair into degeneration.
Lifestyle and targeted interventions to modulate immune activity
You can lower inflammatory burden through concrete steps: 150 minutes/week of moderate aerobic exercise, 5-10% weight loss (often lowering CRP ~20-30%), a Mediterranean-style diet with oily fish twice weekly or 2-3 g/day EPA+DHA, and 7-9 hours sleep. Pharmacologically, short-term NSAIDs or topical steroids control symptoms, while targeted biologics (anti‑TNF, IL‑6 inhibitors, JAK inhibitors) are used in autoimmune disease to markedly reduce systemic cytokines.
Evidence from randomized trials shows these approaches change markers: Mediterranean-style interventions and fish‑oil trials report CRP declines often in the 10-40% range, and exercise protocols (≥150 min/week) typically lower CRP by 10-30%. In inflammatory arthritis, anti‑TNF therapy frequently halves CRP within 8-12 weeks and restores aspects of tissue remodeling. You should time anti-inflammatory use to avoid impairing phases like early bone healing, and combine lifestyle changes with targeted therapy for best outcomes.
Condition 4 – Mitochondrial Health and Metabolic Support
Your cells need mitochondria that both produce ATP efficiently and are regularly renewed through biogenesis and mitophagy; since mitochondria supply roughly 90% of cellular ATP, deficits blunt repair. Stimulating PGC‑1α via targeted exercise, preserving NAD+ pools, and limiting oxidative damage with targeted antioxidants lets mitochondria meet increased energy demands during deep healing, while quality control prevents dysfunctional organelles from generating excess ROS that would stall recovery.
Supporting mitochondrial function – exercise, fuels, NAD+ and antioxidants
You should use a mix of endurance (30-45 min at 60-75% max HR) and 1-2 weekly HIIT or resistance sessions to raise mitochondrial content via PGC‑1α. Favor fuels that support oxidative phosphorylation-fatty acids and ketones-while supplementing NAD+ precursors (NR or NMN in clinical doses like ~250-500 mg/day) and mitochondrial antioxidants such as CoQ10 (100-200 mg/day) or alpha‑lipoic acid to reduce ROS and sustain ATP output.
Promoting metabolic flexibility for energy-efficient repair
Metabolic flexibility – the ability to shift fuel use from glucose (RQ≈1.0) to fat (RQ≈0.7) – speeds healing by matching substrate to demand; interventions like time‑restricted feeding (12-16 hr fast), carb periodization, and regular aerobic/fasted sessions retrain your enzymes and transporters, improving insulin sensitivity and allowing mitochondria to oxidize fat and ketones when needed.
Practically, you can track progress by monitoring fasting glucose, post‑prandial spikes and exercise performance: a flexible metabolism shows lower post‑meal glucose excursions and faster recovery during intervals. Mechanistically, intermittent fasting and exercise activate AMPK and SIRT1, upregulate CPT1 and mitochondrial enzymes, and increase mitochondrial density within 4-12 weeks in sedentary adults. Adopt carbohydrate timing around training (higher carbs on heavy lifting or HIIT days, lower carbs on recovery days), include 30-45 minute fasted aerobic sessions twice weekly, and consider measured NAD+ support and CoQ10 to accelerate shifts; using indirect calorimetry (RQ) or a continuous glucose monitor gives objective feedback on how your metabolism is adapting.
Condition 5 – Clearance, Detoxification, and Mechanical Repair
You must clear metabolic waste and repair mechanical damage before deep healing consolidates; efficient hepatic, lymphatic, and glymphatic flow plus targeted loading prevent persistent inflammation and maladaptive scar, shortening recovery timelines typically seen in 8-12 week rehab programs and improving long‑term tissue quality.
Hepatic, lymphatic, and glymphatic clearance plus hydration basics
Phase I/II liver pathways rely on NADPH and glutathione-N‑acetylcysteine can upregulate GSH-while lymph is propelled by muscle pumps and diaphragmatic breathing; glymphatic clearance peaks during 7-9 hours of slow‑wave sleep and is improved in lateral sleep. Aim for ~30-35 mL/kg/day (≈2.1-2.5 L for 70 kg) and add 20-30 minutes of brisk walking daily to mobilize lymph and support systemic detoxification.
Physical rehabilitation, controlled loading, and tissue remodeling
You should use progressive, tissue‑specific loading: begin with pain‑reducing isometrics, advance to eccentric and heavy‑slow resistance performed about 3×/week, and increase load by roughly 10% per week when tolerated. Clinical trials show heavy‑slow resistance reduces tendinopathy symptoms by ≈50% at 12 weeks, demonstrating how mechanical stimulus orients collagen and restores function.
Start dosing with 45-60 second isometric holds (3×) to blunt nociception, then progress to 3×15 eccentrics and later 3×6-8 heavy reps; use a pain‑monitoring model keeping effort ≤5/10 during sessions and no worsening at 24 hours. Expect collagen synthesis signals in 24-72 hours and remodeling over 3-6 months; combine with NMES, manual therapy, and movement retraining for faster functional gains.
To wrap up
Now that you know the five proven conditions-adequate sleep, balanced nutrition, controlled inflammation, proper hydration, and targeted rest-you can prioritize practices that support cellular repair. By addressing each area, you give your body the environment it needs to initiate deep healing, improve resilience, and sustain long-term recovery.