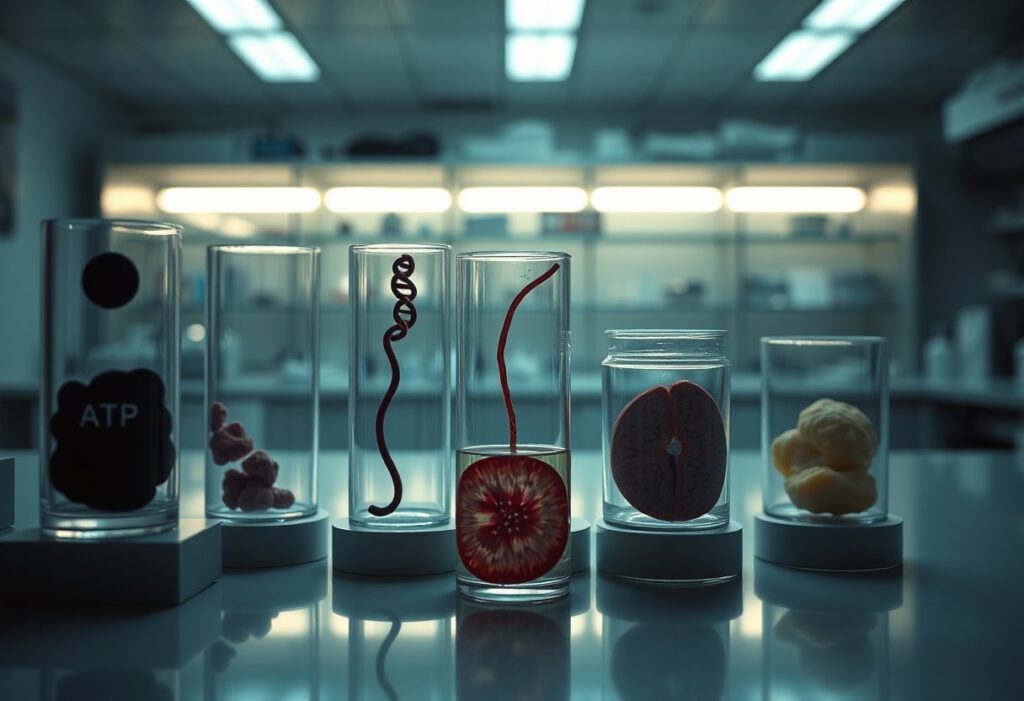
Energy drains when chronic cellular inflammation persists, and you may not realize how profoundly it accelerates aging, saps stamina, disrupts metabolism, impairs cognition, and increases disease risk; this list unpacks ten dangerous long-term effects, explains how inflammation undermines your mitochondria, hormonal balance, immune response, and tissue repair, and shows why addressing inflammation is important to preserve vitality and slow biological aging.
Mitochondrial dysfunction
When chronic inflammation attacks mitochondria, your cellular powerhouses lose efficiency, driving energy deficits and accelerating cellular aging. You experience impaired metabolism, disrupted calcium handling, and poor repair capacity as damaged mitochondria signal for more inflammatory mediators, setting a vicious cycle that undermines tissue function and promotes age-related decline.
Reduced ATP production
Inflammation interferes with oxidative phosphorylation, so your mitochondria produce less ATP and you feel persistent fatigue and reduced physical endurance. Lower ATP impairs cellular maintenance, protein synthesis, and organ function, increasing vulnerability to metabolic disease and slowing recovery from stress or injury.
Increased reactive oxygen species
Inflammatory signaling increases electron leakage in the respiratory chain, raising reactive oxygen species (ROS) that damage lipids, proteins, and DNA. You face amplified oxidative stress that exacerbates mitochondrial injury and promotes further inflammation, creating a self-perpetuating loop that harms cellular function.
Excess ROS from dysfunctional mitochondria oxidize mitochondrial DNA and cardiolipin, impairing ATP synthase and membrane potential; antioxidants like glutathione and superoxide dismutase become depleted, so you lose the capacity to neutralize ongoing oxidative damage. This leads to mutations, activation of inflammasomes, and increased rates of apoptosis and cellular senescence, which collectively contribute to tissue degeneration and the metabolic shifts seen with aging.
Accelerated cellular senescence
Chronic inflammation forces cells into senescence sooner, shortening regenerative capacity and impairing tissue repair; as senescent cells accumulate, they alter metabolism and stress responses, draining your cellular energy and promoting age-related decline in organ function.
Accumulation of senescent cells
Persistent inflammatory signaling increases the pool of non-dividing, dysfunctional cells that you retain in tissues; these cells occupy stem cell niches, secrete damaging factors, and reduce tissue resilience, lowering your ability to replace damaged cells and recover from stress.
SASP promotes tissue dysfunction
The senescence-associated secretory phenotype (SASP) releases pro-inflammatory cytokines, proteases and growth factors that create chronic local inflammation and matrix breakdown, disrupting cell signaling and accelerating functional decline you experience in affected organs.
SASP components degrade extracellular matrix integrity, attract immune cells that sustain inflammation, and induce secondary senescence in neighboring cells, creating a feed-forward loop that undermines mitochondrial function and ATP production, reducing your endurance, repair capacity and cognitive performance over time.
Telomere shortening
You face accelerated telomere shortening when chronic inflammation raises oxidative stress and cell turnover, shaving protective caps at chromosome ends. Shortened telomeres drive genomic instability, impair tissue repair, and sap cellular energy, contributing to faster biological aging and increased disease risk.
Loss of chromosomal protection
Your telomeres normally shield chromosome ends, but inflammation-driven damage accelerates erosion and exposes fragile DNA termini. That loss of protection triggers end-to-end fusions, DNA damage responses, senescence or cell death, undermining genome integrity and long-term tissue function.
Premature cellular aging
You experience premature cellular aging when inflammation-shortened telomeres force cells into senescence or dysfunctional states, reducing proliferation and metabolic capacity. This accelerates tissue decline, impairs repair, and lowers systemic energy availability.
In particular, your senescent cells release the senescence-associated secretory phenotype (SASP), a mix of cytokines and proteases that sustain inflammation, disrupt stem cell niches, and impair mitochondrial function. Over time this feed-forward loop drains your energy reserves, reduces regenerative capacity, and promotes systemic aging and frailty.
Chronic fatigue and reduced stamina
When inflammation becomes chronic, it siphons your cellular energy and undermines endurance: pro-inflammatory cytokines disrupt mitochondrial ATP production, increase oxidative stress, and alter hormonal signals that regulate wakefulness and recovery. The result is persistent tiredness and lowered stamina that accelerates functional decline and makes routine physical tasks feel disproportionately taxing as you age.
Persistent low energy levels
Ongoing inflammation keeps you in a state of metabolic inefficiency, where cytokines interfere with neurotransmitters and sleep architecture, and may promote anemia and insulin resistance. These changes leave you with a steady, low-energy baseline that reduces concentration, motivation, and resilience, eroding daily performance even when you try to rest or conserve energy.
Exercise intolerance and lethargy
Chronic inflammation raises perceived exertion and delays recovery by impairing muscle repair, reducing capillary function, and limiting oxygen delivery, so workouts feel harder and progress stalls. You may pull back from activity to avoid discomfort, which accelerates deconditioning and further entrenches lethargy.
Mechanistically, elevated IL-6, TNF-α and CRP drive mitochondrial dysfunction and muscle catabolism, while autonomic and HPA axis dysregulation blunt cardiovascular responses to exertion; this combination reduces VO2 capacity and fatigue resistance. To break the cycle you need targeted interventions-anti-inflammatory nutrition, graded exercise that respects current tolerance, optimized sleep, and medical assessment for underlying contributors-because addressing inflammation directly restores cellular energy pathways and improves exercise capacity over time.
Insulin resistance and metabolic decline
Chronic inflammation disrupts insulin signaling, causing insulin resistance that reduces your cells’ ability to take up glucose and produce energy, accelerating metabolic decline; over time this drives fatigue, muscle loss, and higher risk of diabetes and age-related metabolic diseases, undermining your vitality and lifespan.
Impaired glucose utilization
Pro-inflammatory cytokines impair insulin receptor signaling and GLUT4 translocation, so your muscles and fat cells can’t efficiently use glucose; your liver compensates by increasing glucose output, raising blood sugar, and forcing energy systems to rely on inefficient pathways that accelerate cellular wear and metabolic aging.
Increased fat accumulation
Persistent inflammation alters adipocyte function and encourages lipogenesis, so you store more fat, particularly visceral fat; inflamed fat secretes more cytokines, creating a self-reinforcing cycle that raises metabolic risk, contributes to insulin resistance, and impairs energy balance.
Inflammation attracts macrophages into fat tissue, forming crown-like structures that amplify cytokine release and alter adipokine profiles-lowering adiponectin and raising leptin and resistin-so your liver and muscle accumulate ectopic lipids, causing lipotoxicity, mitochondrial dysfunction, and systemic insulin resistance that depletes energy and accelerates aging.
Neuroinflammation and cognitive decline
When inflammation becomes chronic in the brain, activated microglia and astrocytes release cytokines that impair neuronal metabolism and synaptic integrity. You lose cognitive reserve as mitochondrial dysfunction and blood-brain barrier breakdown reduce energy supply, slowing processing speed and executive function. Over years this sustained inflammatory milieu accelerates age-related cognitive decline and vulnerability to neurodegenerative disease.
Synaptic dysfunction and memory loss
Persistent inflammatory signals drive excessive microglial pruning and alter neurotransmitter balance, disrupting long-term potentiation necessary for learning. You may notice increased forgetfulness, difficulty forming new memories, and slower retrieval as synapses weaken and neuronal networks lose efficiency. These changes reflect energy deficits at synapses that undermine memory consolidation.
Increased dementia risk
Chronic neuroinflammation elevates your risk of dementia by promoting amyloid accumulation, tau phosphorylation, and vascular injury. Ongoing cytokine exposure and oxidative stress impair clearance mechanisms and accelerate neuronal loss, making cognitive impairment more likely and more severe over time.
At the molecular level, sustained cytokines such as IL-1β and TNF-α hinder microglial phagocytosis and glymphatic clearance of amyloid, while complement-mediated synapse removal and blood-brain barrier permeability permit peripheral immune cells and toxins into brain tissue. You also suffer impaired insulin signaling, mitochondrial dysfunction, and reduced autophagy, compounding energy failure and promoting tau pathology-factors that cumulatively raise dementia risk and can be mitigated by addressing inflammation, metabolic health, sleep, and vascular factors.
Sarcopenia and muscle wasting
Your muscles progressively lose mass and function under chronic inflammation, accelerating sarcopenia and depleting your energy reserves. Persistent cytokine signaling promotes protein breakdown, impairs recovery after stress, and lowers metabolic efficiency, so you age with weaker mobility, slower gait, and greater dependency, undermining resilience to illness and daily activities.
Reduced muscle protein synthesis
Inflammatory cytokines like TNF-α and IL-6 blunt anabolic signaling in your muscle, reducing mTOR activity and diminishing your responsiveness to dietary amino acids and resistance exercise. This shifts the balance toward proteolysis, so you synthesize less muscle protein and struggle to rebuild tissue after injury or inactivity.
Weakness and frailty
As muscle mass falls, you experience measurable weakness: you tire sooner, lose endurance, and move slower, increasing your fall risk and likelihood of losing independence. Chronic inflammation speeds this transition from mild decline to clinical frailty, draining your day-to-day energy and function.
Inflammation also impairs mitochondrial function and neuromuscular junctions, so your remaining muscle performs less efficiently and recovers slowly. You face longer convalescence after illness, higher hospitalization and disability risk, and objective declines in gait speed and grip strength that correlate with elevated inflammatory markers.
Cardiovascular deterioration
Chronic inflammation gradually damages your heart and vessels, causing arterial stiffening, reduced cardiac efficiency, and diminished blood flow to tissues. Over time this inflammation-driven wear increases fatigue, lowers exercise capacity, and accelerates age-related cardiovascular decline that undermines your overall energy and resilience.
Endothelial dysfunction and plaque
Persistent inflammation impairs your endothelial cells’ ability to regulate vessel tone and barrier function, allowing lipids to penetrate the arterial wall. Oxidized LDL and recruited immune cells foster plaque buildup, narrowing arteries and reducing blood delivery to muscles and organs, which drains your energy and raises long-term vascular risk.
Higher heart disease risk
Sustained inflammation increases your likelihood of heart attack, stroke, and heart failure by promoting plaque instability, thrombosis, and adverse cardiac remodeling. Elevated inflammatory markers correlate with higher event rates, meaning ongoing immune activation directly translates into greater cardiovascular danger for you.
Mechanistically, inflammation enhances coagulation, weakens fibrous caps on plaques, and provokes arrhythmogenic remodeling of heart tissue, so a small plaque can suddenly cause a major blockage. Monitoring inflammatory markers and addressing chronic inflammatory drivers can reduce the cumulative vascular damage that puts your heart at risk.
Immune senescence and infection
As immune cells age, your defenses weaken, raising risk of infections and poorer vaccine responses. Senescent immune cells secrete inflammatory mediators that sap energy, impede tissue repair, and shift resources toward chronic inflammation, accelerating biological aging and reducing your resilience to new challenges.
Poor pathogen clearance
When immune senescence reduces pathogen recognition and clearance, you endure longer, more severe infections and repeated inflammatory flares. Diminished T cell responses and impaired phagocytosis allow microbes to persist, forcing your system into frequent high-energy immune activity that depletes metabolic reserves.
Chronic low-grade infections
Low-grade infections that smolder in tissues generate continuous antigen exposure; you might not have obvious illness, yet ongoing immune activation drives fatigue and muscle breakdown. Persistent cytokine release from these infections contributes to cumulative tissue damage and hastens aging-related functional decline.
Chronic low-grade infections often involve intracellular pathogens, biofilm-associated bacteria, or reactivating viruses like herpes; you may notice subtle signs-persistent fatigue, low-grade fever, or brain fog. These infections sustain cytokines (IL-6, TNF-α) that impair mitochondrial ATP production. Detecting them requires sensitive diagnostics and attention to risk factors, while management typically pairs targeted antimicrobials with immune-supportive and anti-inflammatory strategies to help restore your metabolic balance.

Impaired autophagy and proteostasis
When autophagy and proteostasis falter, your cells cannot clear misfolded proteins and damaged organelles, leading to metabolic inefficiency and chronic cellular stress. Inflammation inhibits autophagic signaling and proteasome activity, which lowers ATP production, increases oxidative damage, and accelerates cellular aging processes that sap your energy and resilience.
Accumulation of damaged proteins
Chronic inflammation disrupts chaperones and the ubiquitin-proteasome system, allowing misfolded and oxidized proteins to build up in your cytoplasm. This proteotoxic load impairs signaling and membrane function, stresses mitochondria, and drives cells toward senescence, reducing tissue performance and contributing to fatigue and age-related decline.
Reduced cellular cleanup
Inflammation-driven suppression of autophagy impairs your cells’ ability to remove dysfunctional mitochondria and protein aggregates, lowering energy output and increasing reactive oxygen species. Over time, reduced cellular cleanup undermines stem cell function and immune surveillance, making tissues less adaptable and more susceptible to degenerative conditions.
At a molecular level, inflammatory pathways such as sustained mTOR activation and NF-κB signaling inhibit autophagosome formation and lysosomal degradation, while p62/SQSTM1 accumulates and further disrupts proteostasis. Impaired mitophagy leaves you with inefficient mitochondria, manifesting clinically as chronic fatigue, muscle wasting, cognitive decline, and heightened vulnerability to metabolic and neurodegenerative diseases.
Conclusion
On the whole you should view chronic cellular inflammation as a persistent drain that accelerates aging, saps energy, impairs cognition, disrupts metabolism, increases disease risk, and undermines recovery and resilience; addressing inflammation through lifestyle, targeted medical care, and monitoring helps you preserve your mitochondrial function, maintain vitality, and reduce long-term morbidity so you can age healthier and retain functional capacity.