Influence Hormones
Many metabolic processes depend on cellular nutrition, and understanding six critical nutrition signals-energy status, amino acid availability, fatty acid signaling, micronutrient cofactors, oxidative balance, and hormonal feedback-helps you influence hormone function and tissue repair, and lets you shape your diet and timing to support recovery, optimize metabolic resilience, and reduce inflammation for better long-term health outcomes.
Table of Contents
Cellular Nutrition Fundamentals
Your cells translate the food you eat into signaling inputs that steer growth, metabolism, and repair; amino acids (especially leucine), glucose, fatty acids, and micronutrients act as distinct ligands that modulate signaling hubs, redox state, and cofactor availability, so altering meal timing, macronutrient ratios, or micronutrient status shifts hormone responses and repair programs within hours to days and influence hormones.
Nutrient transport and intracellular sensing
You control flux into cells through transporters like GLUTs for glucose, LAT1 and SNATs for amino acids, and CD36/FATP for fatty acids; intracellular sensors such as Sestrin2 (leucine), CASTOR1 (arginine) and SAMTOR (SAM) convey substrate levels to mTORC1 via Rag GTPases and lysosomal recruitment, while rapid transporter trafficking (e.g., insulin-driven GLUT4 translocation in 10-20 minutes) tunes acute signaling.
Core signaling hubs: mTOR, AMPK, insulin/IGF pathways
You face a balance where mTORC1 drives protein synthesis and lipid anabolism when amino acids and growth factors are high, AMPK activates under low ATP to switch on catabolism and inhibit mTOR, and insulin/IGF signaling (PI3K→Akt) amplifies anabolic programs and suppresses FOXO-mediated catabolic genes, producing integrated growth versus repair decisions across tissues and influence hormones.
You can trace molecular detail: mTORC1 activation requires amino-acid-dependent Rag GTPase recruitment to the lysosomal surface plus Rheb-GTP, while AMPK is phosphorylated at Thr172 (by LKB1 or CaMKKβ) when AMP/ADP rise, and insulin/IGF produce PIP3 to recruit PDK1/Akt-Akt then phosphorylates TSC2 and PRAS40 to relieve mTORC1 inhibition; downstream, S6K and 4E-BP1 control translation and cell size.
Cellular repair mechanisms: autophagy, proteostasis, DNA repair
You rely on autophagy to clear damaged organelles, the ubiquitin-proteasome system plus chaperones (HSP70, HSP90) to maintain proteostasis, and multiple DNA-repair pathways-BER, NER, mismatch repair, and DSB repair (NHEJ/HR)-to fix lesions; nutrient and energy status directly modulate these systems via mTOR, AMPK, NAD+ and sirtuin signaling and influence hormones..
Nutrient signals interact with repair machinery: mTOR inhibition (fasting, rapamycin) increases LC3 lipidation and autophagosome formation, PINK1-Parkin mediates mitophagy for dysfunctional mitochondria, the ER UPR (PERK/IRE1/ATF6) handles misfolded proteins, and NAD+-dependent PARP/sirtuins support base-excision and double-strand-break repair-supplementation that raises NAD+ (e.g., NR) has improved DNA repair metrics in mouse studies.
Nutrition-to-Hormone Communication
Nutrition-to-hormone communication is the body’s real-time control system for deciding what to do with incoming energy and building blocks. The moment you eat, nutrients aren’t just “fuel”; they become signals. Carbohydrates raise blood glucose and, almost immediately, your gut releases incretin hormones such as GLP-1 and GIP. These incretins amplify the pancreas’ insulin response even before blood sugar peaks, which is why the gut matters so much in metabolic control and influence hormones.
As glucose enters the bloodstream, insulin rises to coordinate storage and usage: it tells muscle and fat cells to pull glucose in, tells the liver to reduce glucose output, and sets a short-term “anabolic and organize resources” program and influence hormones.. In many people, post-meal insulin reaches a high point roughly 30–60 minutes after eating, but the shape of that curve is heavily influenced by meal composition—fiber and protein slow absorption, while refined carbs and liquid sugars tend to accelerate it.
Protein signals growth and repair through amino acids—especially leucine, where about 2–3 g per meal can strongly trigger mTORC1 and muscle protein synthesis, with training making muscles more responsive and insulin helping reduce breakdown. Fats signal through fatty-acid and bile-acid pathways (PPARs and FXR), shaping how you burn or store energy and affecting satiety beyond just “slow digestion.” Your gut also releases hormones (GLP-1, GIP, CCK, PYY, ghrelin) that quickly influence insulin, hunger, fullness, and gastric emptying, so meals with the same calories can feel very different. Fiber adds a slower signal via gut microbes and short-chain fatty acids, supporting longer-lasting satiety and metabolic health and influence hormones..
Acute vs. chronic nutrient signaling and endocrine responses
Acute nutrient signals-postprandial insulin spikes, transient GLP-1 surges, AMPK activation during fasting-drive short-term recovery and storage, whereas chronic overexposure to high-glycemic meals or excess calories promotes sustained hyperinsulinemia, receptor desensitization, and insulin resistance over weeks to months. You can observe reversal with interventions: time-restricted eating or reduced refined carbohydrate intake often improves insulin sensitivity within 4-12 weeks in controlled trials and influence hormones..
Inflammation, immune signaling, and hormonal cross-talk
Pro-inflammatory cytokines (TNF-α, IL-6) and acute-phase proteins (hs-CRP) directly interfere with insulin and steroid signaling by promoting serine phosphorylation of IRS proteins and altering aromatase activity, so your immune state reshapes metabolic and reproductive hormones. Low-grade inflammation is clinically evident when hs-CRP is in the 2-10 mg/L range, and visceral adipose secretes adipokines that amplify this hormonal disruption.
In practical terms, reducing inflammation improves hormonal profiles: a 5-10% weight loss typically lowers hs-CRP and IL-6 and restores insulin responsiveness, and targeted nutrients-omega-3s (1-3 g EPA+DHA/day) or polyphenols like curcumin-have shown CRP reductions in randomized trials. You should consider both dietary composition and anti-inflammatory strategies to break the feedback loop between immune signaling and endocrine dysfunction.
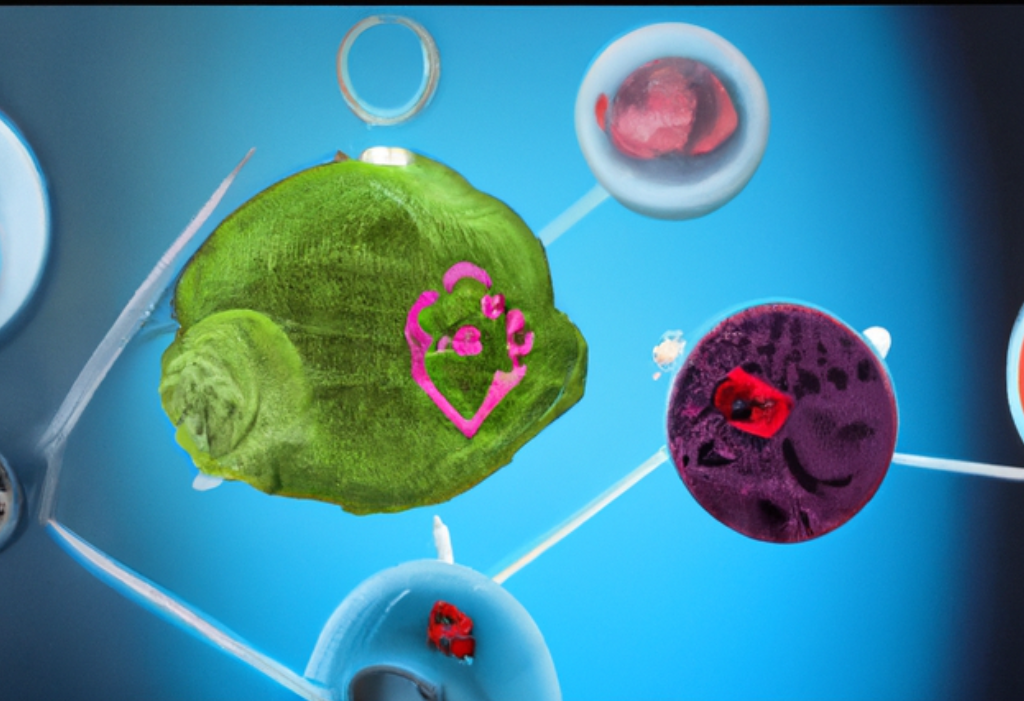
The 6 Critical Nutrition Signals That Influence Hormones and Repair
You’ll find six nutrition-driven signals that steer hormone networks and tissue repair, each altering signaling cascades, transcription factors, and metabolic fluxes; together they set anabolic or catabolic states, shift inflammation, and determine repair efficiency, with measurable biomarkers (glucose 70-140 mg/dL, 25(OH)D ng/mL, ketones 0.5-3 mmol/L) to guide interventions and influence hormones.
Glucose/insulin and energy availability
You rely on glucose and insulin as rapid toggles for growth versus conservation: postprandial insulin promotes GLUT4 uptake, glycogen synthesis and mTOR activation, while low glucose activates AMPK and autophagy; for example, keeping post-meal glucose below ~140 mg/dL limits glycation and preserves repair signaling, and intermittent low-energy periods boost repair through AMPK-driven pathways.
Branched-chain and vital amino acids – mTOR/IGF-1 activation
You trigger mTORC1 most potently with leucine-about 2-3 g per meal-so a 20-30 g whey serving gives you a strong anabolic signal that raises muscle protein synthesis and IGF-1 signaling; frequent high-protein feeding sustains mTOR, suppresses autophagy, and accelerates structural repair when you need growth.
You should note that mTORC1 senses amino acids at the lysosomal surface via sensors like Sestrin2 and CASTOR, with leucine and arginine recruiting Rag GTPases; this suppresses ULK1-driven autophagy and increases ribosomal biogenesis, so timing (post-exercise protein) and dose (20-40 g protein with ~2-3 g leucine) determine whether you favor net synthesis versus clearance and influence hormones..
Fatty acids and lipid mediators (omega-3s, eicosanoids)
You modulate inflammation and hormone output through fatty-acid-derived mediators: EPA/DHA (1-3 g/day) produce anti-inflammatory resolvins, while arachidonic acid yields pro-inflammatory prostaglandins; shifting substrate availability changes COX/LOX-derived eicosanoid profiles and impacts insulin sensitivity, steroidogenesis, and membrane receptor function.
You can alter signaling by changing tissue fatty-acid composition-EPA competes with arachidonic acid for COX/LOX, lowering PGE2 and leukotriene B4 synthesis; given a typical Western omega-6:omega-3 ratio of 10-20:1, moving toward 4:1 or lower improves membrane fluidity, PPAR activation, and downstream gene expression tied to repair and metabolic resilience.
Micronutrients and cofactors (vitamin D, zinc, magnesium)
You depend on specific micronutrients as enzyme cofactors and transcriptional modulators: vitamin D status (25(OH)D >30 ng/mL) tunes immune and repair gene expression, zinc (8-11 mg/day) stabilizes insulin and DNA-repair enzymes, and magnesium (310-420 mg/day) is vital for ATP-dependent kinases; deficiencies blunt hormone signaling and slow tissue repair.
- Vitamin D modulates VDR-driven transcription in immune and muscle cells.
- Zinc is required for metalloproteases and antioxidant enzymes involved in healing.
- Magnesium supports ATP, kinase activity, and DNA repair.
- Assume that these cofactors interact-deficiency in one often impairs pathways supported by the others.
You should screen and correct common insufficiencies because each micronutrient alters repair kinetics: vitamin D supplementation (1,000-4,000 IU/day) raises VDR activity, zinc (10-30 mg short-term) restores immune function, and magnesium (200-400 mg/day) improves glucose handling and kinase reactions; testing guides dosing to avoid excess and ensure effective hormonal and repair responses and influence hormones.
- Test 25(OH)D, serum zinc, and ionized magnesium when repair or hormonal dysfunction persists.
- Adjust supplementation based on levels, comorbidities, and drug interactions.
- Assume that correcting one deficiency may reveal another-monitor and retest.
Ketone bodies and fasting/AMPK-SIRT signaling
You activate AMPK and sirtuins during fasting or ketogenic states: β-hydroxybutyrate (BHB) at 0.5-3 mmol/L serves as both fuel and HDAC inhibitor, raising NAD+/NADH ratio, promoting mitochondrial biogenesis via PGC-1α, and increasing autophagy-approaches like 16:8 intermittent fasting or low-carb diets shift you into this repair-promoting signaling milieu.
You can harness BHB’s signaling beyond energy: it inhibits class I HDACs to de-repress FOXO and antioxidant genes, increases SIRT1/3 activity to promote mitochondrial quality control, and synergizes with AMPK to induce mitophagy; achieving sustained mild ketosis (0.5-1.5 mmol/L) through dietary timing or exogenous ketones produces reproducible effects on metabolic and neuronal repair.
Gut-derived metabolites and bile acids (SCFAs, microbial signals)
You receive signals from microbiota-produced metabolites-acetate, propionate, and butyrate at millimolar concentrations in the colon activate GPR41/43, increase GLP‑1/PYY, and modulate hepatic glucose output; bile acids acting via FXR and TGR5 alter FGF19 and insulin sensitivity, so dietary fiber and microbiome composition directly influence hormonal and repair pathways and influence hormones..
You should note functional outcomes: butyrate fuels colonocyte repair and tight-junction integrity, propionate informs hepatic gluconeogenesis and appetite circuits, and secondary bile acids remodel FXR signaling to change lipid and glucose homeostasis; interventions like 20-30 g/day fermentable fiber or targeted probiotics reliably raise SCFA output and improve hormonal repair markers in weeks.
Tissue Repair Outcomes and Hormonal Modulation
Hormonal milieu dictates whether your tissues rebuild efficiently or stall in chronic damage: insulin and IGF-1 activate mTOR to favor synthesis, while persistent cortisol and pro-inflammatory cytokines drive proteolysis and extracellular matrix breakdown. You should prioritize timed protein (20-40 g leucine-rich per meal), glycemic control, and sleep to keep anabolic windows open and support effective collagen deposition and cellular turnover during repair and influence hormones.
Muscle and connective tissue repair: anabolic vs. catabolic balance
You depend on anabolic signals-insulin/IGF-1, testosterone, and estrogen-to stimulate muscle protein synthesis and tendon collagen formation; target 1.2-1.6 g/kg protein daily, distribute 20-40 g servings every 3-4 hours, and perform resistance training 2-3 times per week to maximize MPS. In contrast, chronic cortisol elevation from stress or prolonged high-intensity endurance sessions (>60 minutes) shifts you toward catabolism, increasing proteolysis and delaying ligament and tendon remodeling unless anabolic input is restored.
Wound healing, neurorepair, and metabolic resilience
Wound closure and neurorepair require a coordinated inflammatory phase, angiogenesis (VEGF), and matrix remodeling driven by TGF-β and M2 macrophages; the M1→M2 transition typically occurs around days 3-7. You improve outcomes by keeping glucose under ~180 mg/dL, supplying 20-40 g protein per meal (higher-~1.5 g/kg-if catabolic), and using 20-40 minute aerobic sessions to elevate BDNF for neural recovery; stimulating AMPK/PGC-1α via exercise or 12-16 hour fasting boosts mitochondrial resilience and influence hormones..
If you experience a skin or nerve injury, expect angiogenesis and early collagen deposition within 7-14 days, so maintain consistent protein and euglycemia to support matrix synthesis; in catabolic or infected states increase protein toward 1.5 g/kg. Supplementing omega‑3s (1-2 g/day EPA+DHA) can reduce excessive inflammation, while progressive aerobic plus resistance training enhances BDNF and mitochondrial biogenesis, lowering fibrosis risk and improving functional neurorepair metrics such as strength and sensory recovery and influence hormones.
Practical Dietary and Timing Strategies
You can optimize hormone signaling and repair by pairing macronutrient targets with consistent meal timing, aligning larger carbohydrate loads to active periods and concentrating protein around workouts and sleep. Aim to spread intake across the day so anabolic signals occur repeatedly rather than in a single surge; combine resistance training with post-exercise protein and carbohydrates to amplify insulin- and mTOR-mediated repair pathways and influence hormones..
Macronutrient composition, protein timing, and feeding patterns
You should target 1.2-1.6 g/kg/day of protein (athletes up to 2.0 g/kg), delivering ~20-40 g of high-quality protein every 3-4 hours to hit the ~2.5 g leucine threshold per meal for muscle protein synthesis. Pair 0.3-0.6 g/kg carbs within 30-60 minutes post-exercise when rapid glycogen restoration matters, and consider an 8-10 hour time-restricted feeding window if reducing late-night insulin spikes and improving circadian alignment is a goal and influence hormones.
Targeted micronutrient interventions and supplementation guidance
You should base supplementation on labs and symptoms: vitamin D3 commonly 1,000-4,000 IU/day to reach 30-50 ng/mL, magnesium 200-400 mg at night for sleep and recovery, omega-3 EPA+DHA 1-3 g/day for anti-inflammatory effects, zinc 15-30 mg short-term for immune support, and iron only when ferritin/hemoglobin indicate deficiency. Test levels, dose appropriately, and adjust after 8-12 weeks rather than guessing and influence hormones.
Further practical steps include taking fat-soluble supplements (vitamin D, omega-3s) with a meal containing fat to improve absorption, spacing zinc or iron away from calcium and high-fiber meals to avoid interaction, and preferring chelated magnesium forms (glycinate) to reduce GI upset. You can follow a simple protocol: baseline labs (vitamin D, ferritin, CRP, magnesium if possible), targeted replenishment based on ranges, then recheck after 8-12 weeks to titrate dosing and avoid chronic excessive intakes and influence hormones.
Monitoring and Clinical Application
Use serial, time‑bound measurements to guide interventions and titrate nutrients: baseline labs, then reassess at 4-12 weeks for metabolic signals and again at 6 months for repair outcomes. You’ll combine static markers (HbA1c, fasting insulin) with dynamic tools (CGM, OGTT, indirect calorimetry) and symptom tracking to link dietary or supplement changes to hormonal shifts, inflammation, and tissue recovery, adjusting dose, timing, or macronutrient balance based on objective trends rather than single measurements and influence hormones.
Biomarkers and functional tests to assess signaling and repair
Prioritize insulin/glucose metrics (fasting insulin, HOMA‑IR, HbA1c, 2‑hr OGTT, CGM), inflammatory markers (hs‑CRP, IL‑6), lipid ratios (TG/HDL), 25(OH)D (target 30-50 ng/mL), omega‑3 index (>8% ideal), intracellular magnesium and RBC folate, thyroid panel including free T3, sex hormones (total/free testosterone, estradiol, SHBG), and urine organic acids or metabolomics for mitochondrial function; reserve phospho‑protein assays or telomere/γH2AX testing for research or complex cases.
Personalization by age, sex, metabolic phenotype, and comorbidities
Tailor targets and interventions: older adults often need higher protein (1.2-1.5 g/kg) and vitamin D for repair, women with PCOS need strategies emphasizing insulin lowering and anti‑inflammatory fats, APOE4 carriers limit saturated fat and monitor lipids more frequently, and you’ll alter macronutrient ratios or supplement dosing in renal, hepatic, or autoimmune disease to avoid harm while optimizing signaling and influence hormones.
For practical application, map phenotype to protocol: if a patient has HOMA‑IR >2.5 and postprandial glucose excursions on CGM, you’ll prioritize carbohydrate timing, incremental resistance exercise, and low‑GI Mediterranean patterns; if frail and sarcopenic, increase protein, leucine‑rich sources, and monitor creatinine, albumin, and function every 6-12 weeks to confirm anabolic response and adjust calories to support repair without exacerbating comorbidity and influence hormones.
Final Words
Drawing together the insights on cellular nutrition, you see how six targeted signals-macronutrient balance, micronutrient sufficiency, energy timing, hydration, inflammatory control, and mitochondrial support-shape your hormonal landscape and drive tissue repair and influence hormones. By aligning your diet and lifestyle to modulate these pathways, you optimize hormone signaling, accelerate recovery, and sustain cellular resilience for long-term health and influence hormones.