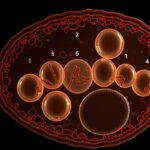
Most of your recovery depends on signals from repair hormones; this post outlines seven powerful cues-growth factor pulses, sleep-related melatonin peaks, anti-inflammatory shifts, metabolic resets, stem-cell activation, vascular repair signals, and hormonal balance-that drive regeneration, how they work, and practical steps you can take to optimize them for faster healing and deeper restoration.
Key Takeaways:
- Growth hormone (GH) – drives cell proliferation, collagen synthesis and stem-cell activation for tissue repair, peaking during deep sleep and fasting.
- Insulin-like growth factor 1 (IGF-1) – mediates GH effects, promotes muscle regeneration and protein synthesis at injury sites.
- Melatonin – coordinates circadian repair, enhances antioxidant defenses and mitochondrial recovery during sleep.
- Testosterone – supports muscle rebuilding, protein anabolism and satellite cell activity after stress or injury.
- Estrogen – modulates inflammation, protects tissues and enhances extracellular matrix remodelling in recovery.
- Insulin – facilitates nutrient uptake and anabolic signaling that fuels repair and glycogen replenishment.
- Vascular endothelial growth factor (VEGF) – stimulates angiogenesis to restore blood flow and nutrient delivery to healing tissues.
Understanding Repair Hormones
Your body’s repair network is time‑dependent and hormone‑driven: inflammatory prostaglandins spike within minutes, growth hormone surges during deep sleep to enhance tissue synthesis, and IGF‑1 sustains cell proliferation over days. You experience coordinated phases-acute inflammation, proliferation, remodeling-each regulated by different endocrine signals so that protein synthesis, immune resolution, and matrix rebuilding occur in the right sequence for effective recovery.
The Role of Hormones in the Healing Process
Hormones act as on/off switches and modulators: cortisol tempers inflammation, insulin delivers nutrients to rebuilding cells, and thyroid hormones set metabolic pace. You rely on pulsatile growth hormone-largest pulse in the first 90 minutes of sleep-to trigger anabolic pathways, while melatonin and estrogen influence antioxidant defenses and vascular repair, shaping both speed and quality of healing.
Key Hormones Involved in Regeneration
Major players include growth hormone (GH), IGF‑1, insulin, testosterone, estrogen, cortisol, thyroid hormones, and melatonin. You see GH/IGF‑1 drive cell proliferation, insulin support substrate uptake, sex hormones modulate fiber and tendon repair, and cortisol balance inflammation versus tissue synthesis-each hormone contributing distinct, measurable effects during different recovery windows.
GH is secreted in pulses roughly every 3-4 hours with the largest nocturnal surge; that GH stimulates hepatic IGF‑1 production, which promotes satellite cell proliferation. Insulin spikes post‑meal to refill glycogen and amino acid pools, while excess cortisol (chronically elevated) can reduce collagen synthesis by up to an estimated 20-30% in prolonged stress models. Estrogen enhances angiogenesis and limits fibrosis, and melatonin preserves mitochondrial function during regeneration.
The Seven Powerful Signals
These seven hormones act as timing and intensity cues for tissue repair: growth hormone pulses during slow‑wave sleep, testosterone peaks in the morning and after heavy lifts, IGF‑1 (extended half‑life via IGFBPs) drives local growth, cortisol follows a diurnal curve and spikes with prolonged stress, estrogen modulates collagen and inflammation across the menstrual cycle, thyroid hormones set metabolic throughput, and progesterone shapes immune tone and sleep-together they determine whether you rebuild stronger or stall.
Signal 1: Growth Hormone
Growth hormone (GH) surges in deep sleep and after high‑intensity exercise, with a plasma half‑life around 20-30 minutes; it stimulates IGF‑1 production, increases amino acid uptake and protein synthesis, and promotes lipolysis, so when you optimize slow‑wave sleep and sprint or heavy resistance sessions you amplify GH‑driven repair.
Signal 2: Testosterone
Testosterone supports muscle protein synthesis, satellite cell activation and neuromuscular recovery; males typically range ~300-1,000 ng/dL total, with only 1-3% free, and you’ll see short‑term rises after compound resistance work and declines with age (~1%/year after 30) that slow regenerative capacity.
Practically, you can boost reparative testosterone signals by prioritizing morning resistance sessions and sleep-acute lifts raise levels for 15-60 minutes, while chronic sleep loss and high cortisol lower free testosterone; monitoring the testosterone:cortisol ratio gives you a simple recovery metric after intense training blocks.
Signal 3: Insulin-like Growth Factor (IGF)
IGF‑1, largely produced in the liver in response to GH but also expressed locally in muscle, mediates anabolic effects and cell proliferation; bound to IGFBPs it enjoys a 12-15 hour effective lifespan, so when you stimulate muscle (especially eccentrics) you trigger sustained IGF signaling that drives repair.
Local IGF‑1 isoforms, like mechano growth factor (MGF), spike within hours after eccentric loading and activate satellite cells; older adults show blunted MGF responses, explaining slower recovery, while nutrition (adequate protein and leucine) amplifies IGF‑driven synthesis during the 24-48 hour repair window.
Signal 4: Cortisol
Cortisol mobilizes glucose, limits excessive inflammation and aids early wound‑cleaning, peaking in the morning (typically 7-9 AM) and rising with prolonged exercise or stress; short elevations help, but sustained high cortisol impairs collagen deposition and muscle protein balance, so you must balance stressors and recovery.
The cortisol:testosterone ratio is a practical recovery indicator-elevated cortisol from sleep deprivation or chronic overtraining (even a single night of restricted sleep can raise evening cortisol ~15-25%) shifts you toward catabolism and slows tendon and muscle healing unless you reduce load and restore sleep.
Signal 5: Estrogen
Estrogen modulates inflammation, enhances collagen synthesis and tendon stiffness, and protects muscle from damage; cyclic fluctuations mean your repair capacity changes across the menstrual cycle, with many women experiencing altered soreness and connective‑tissue responses between follicular and luteal phases.
Evidence shows estrogen replacement in postmenopausal women reduces exercise‑induced muscle damage markers (e.g., lower creatine kinase) and improves collagen turnover; when you account for cycle phase or hormonal status you can time higher‑load sessions to windows with more favorable tendon and muscle remodeling.
Signal 6: Thyroid Hormones
Thyroxine (T4) and triiodothyronine (T3) set basal metabolic rate, mitochondrial activity and protein turnover; adequate thyroid signaling speeds cellular energy supply for repair, whereas hypothyroid states slow wound healing, reduce collagen synthesis and blunt exercise recovery rates.
In acute illness or severe stress you often see “low T3 syndrome,” which correlates with poorer recovery; optimizing thyroid function (euthyroid range TSH and normal free T3/T4) supports mitochondrial biogenesis and ATP production crucial for tissue regeneration and rehabilitation progress.
Signal 7: Progesterone
Progesterone modulates immune responses, has anti‑inflammatory and neuroprotective actions, and raises basal body temperature by ~0.3-0.5°C in the luteal phase, which alters thermoregulation and perceived exertion-these effects influence how you recover from both musculoskeletal and neural insults.
Metabolites like allopregnanolone enhance GABAergic tone, improving sleep quality and potentially accelerating neural repair; however, high progesterone can slightly blunt anabolic signaling, so consider cycle phase when planning heavy training or rehabilitation to align immune and hormonal environments for optimal recovery.
Factors Influencing Hormonal Signals
Multiple variables determine how effectively your repair hormones fire: age (testosterone declines roughly 1% per year after 30), circadian timing (deep sleep drives most nightly GH release within the first 90 minutes), and medication exposure (glucocorticoids blunt inflammation and tissue rebuilding). Genetic variance and environmental toxins shift baseline set points, while acute behaviors – meals, training, stress spikes – modulate hourly pulses. After prolonged caloric deficit or chronic sleep restriction your repair hormones downregulate and recovery lengthens.
- Sleep quality and timing
- Macronutrients, micronutrients
- Exercise type and intensity
- Psychosocial stress and allostatic load
- Medications, alcohol, environmental toxins
- Age, sex, genetic predisposition
- Circadian alignment and light exposure
Nutrition and Its Impact on Hormone Production
Your food choices directly alter hormone availability: 20-30 g of protein per meal with ~2.5 g leucine triggers muscle protein synthesis via mTOR/IGF‑1, while omega‑3s (1-3 g/day) lower pro‑inflammatory eicosanoids. Vitamin D and zinc deficiencies suppress testosterone and wound healing, and repeated high‑glycemic meals drive insulin spikes that blunt autophagy and shift repair toward fat storage rather than tissue regeneration.
Lifestyle Choices and Hormonal Balance
How you move, sleep, and manage stress reshapes hormonal signaling: resistance training sessions (2-4×/week) produce acute testosterone and GH surges; 20-30 minutes of HIIT elevates catecholamines and mitochondrial biogenesis; chronic psychological stress raises baseline cortisol and inflammatory cytokines, impairing recovery capacity and tissue repair.
Shift work or erratic sleep timing suppresses melatonin and disrupts cortisol rhythms, reducing nocturnal GH peaks; practical measures like a fixed sleep window (7-9 hours), avoiding caffeine 6+ hours before bed, and scheduling intense training earlier in the day preserve circadian hormone patterns and accelerate regeneration.
Strategies to Optimize Repair Hormones
Targeted habits amplify your repair-hormone signals: resistance training can raise growth-hormone pulses up to 200% post-session, intermittent fasting shifts nocturnal GH timing, and 20-40 minutes of HIIT acutely increases catecholamines to prime remodeling; combine consistent sleep, strategic protein timing, and periodized stress to convert these acute spikes into sustained regenerative gains.
Exercise and Physical Activity
Prioritize progressive overload with 2-3 resistance sessions weekly (3-5 sets of 6-12 reps for major lifts) and include eccentric-focused sets to boost satellite cell activation; add 1-2 sprint or HIIT sessions to spike GH and catecholamines, plus 2 sessions of 30-60 minutes low-intensity work per week to promote mitochondrial biogenesis and recovery capacity.
Sleep and Recovery Techniques
Optimize sleep duration and timing: aim for 7-9 hours nightly, keep bedtime within ±30 minutes across days, and avoid screens 60-90 minutes before bed so you maximize slow-wave sleep-the phase that produces the largest GH pulse in the first 60-90 minutes after sleep onset; maintain bedroom temperature around 16-19°C for better sleep efficiency.
Further enhance overnight repair by taking 20-40 g casein protein 30 minutes before bed to elevate overnight muscle protein synthesis, using 20-30 minute midday naps if nightly sleep is short, and dimming lights in the evening to boost melatonin; track deep-sleep percentage and aim for roughly 15-25% of total sleep to support anabolic and cognitive recovery.
Common Misconceptions About Repair Hormones
Too often you’ll hear hormones framed as single-purpose fixes or magic bullets; in reality they act as time‑coded signals whose effects depend on dose, pattern and tissue context. For example, growth hormone is released in pulsatile surges-primarily in the first 90 minutes of deep sleep-so bluntly boosting circulating levels without restoring sleep architecture won’t replicate natural repair. Historical shifts like the WHI findings on estrogen show how outcome depends on timing, formulation and patient phenotype, not just “hormone replacement” as a monolith.
Myths Surrounding Hormonal Treatments
You may be told that replacing a hormone always restores function or that higher levels equal faster repair; both are misleading. Exogenous testosterone can suppress spermatogenesis by lowering intratesticular testosterone, while chronic supraphysiologic glucocorticoids produce muscle wasting and HPA axis suppression. Clinical outcomes hinge on regimen, route and monitoring-transdermal versus oral estrogens have different hepatic effects-so broad claims about safety or universal benefit are often wrong.
Clarifying Hormonal Function in Recovery
Hormones operate as contextual messengers: timing, pulsatility and receptor sensitivity shape outcomes more than absolute concentration. Cortisol follows a diurnal peak within ~30-45 minutes after waking that mobilizes energy, whereas GH pulses during early slow‑wave sleep drive nocturnal anabolic processes; disrupting those patterns-say, by shift work or sleep loss-blunts repair even if blood levels appear “normal.”
Practically, you see this in exercise recovery: resistance training triggers transient rises in testosterone and GH that, together with elevated muscle protein synthesis, promote adaptation over the next 24-48 hours; conversely, a night of poor sleep reduces GH pulsatility and increases catabolic cortisol, extending recovery time and impairing strength gains. Monitoring timing and restoring rhythms often yields bigger benefits than isolated hormone supplementation.
To wrap up
With these considerations you can harness Repair Hormones – 7 Powerful Signals That Trigger Regeneration and Deep Recovery to optimize your healing and performance. By tracking and supporting the seven signals through sleep, nutrition, targeted movement, and stress management, you give your body the environment it needs to regenerate efficiently, reduce downtime, and sustain long-term resilience.
FAQ
Q: What are repair hormones and how do they support regeneration?
A: Repair hormones are signaling molecules-like growth hormone, insulin-like growth factor 1 (IGF-1), melatonin, testosterone, estrogen, cortisol (in controlled pulses), and thyroid hormones-that coordinate cellular repair, tissue rebuilding, inflammation resolution, and metabolic shifts favoring recovery. They regulate stem cell activation, protein synthesis, antioxidant defenses, and removal of damaged components through autophagy, enabling structural and functional restoration after injury, stress, or daily wear.
Q: Which seven signals trigger deep recovery and how do they work together?
A: The seven key signals commonly highlighted are: growth hormone (stimulates tissue synthesis and fat metabolism), IGF-1 (amplifies growth hormone effects and promotes cell proliferation), melatonin (resets circadian rhythms and enhances antioxidant activity), testosterone/estrogen (support muscle and connective tissue repair and influence inflammation), cortisol rhythm (short-term rises mobilize energy; low nocturnal levels favor repair), thyroid hormones (regulate metabolic rate for repair), and anti-inflammatory cytokines (resolve inflammation and permit regeneration). They interact via feedback loops: sleep-dependent melatonin boosts growth hormone release; sex steroids modulate IGF-1 and inflammatory responses; thyroid status sets metabolic capacity. Balanced timing and amplitude of each signal allow coordinated healing rather than prolonged inflammation or catabolism.
Q: What lifestyle practices reliably enhance these repair signals?
A: Prioritize consistent sleep timing and quality to optimize melatonin and growth hormone pulses; practice resistance training and adequate progressive overload to stimulate IGF-1 and anabolic pathways; ensure sufficient protein and micronutrients (vitamin D, zinc, magnesium) to support hormone production and tissue synthesis; use time-restricted eating or short fasting windows strategically to enhance autophagy and insulin sensitivity; manage stress with breathing, meditation, or brief aerobic exercise to preserve healthy cortisol rhythms; and maintain healthy body composition and moderate alcohol intake to sustain sex steroid and thyroid function.
Q: How can I tell if my repair signaling is impaired?
A: Common signs include poor sleep and daytime fatigue (blunted melatonin/growth hormone cycles), slow wound healing or persistent soreness (reduced anabolic signaling), chronic low-grade inflammation or frequent infections (imbalanced cytokines and cortisol), muscle loss or difficulty building strength (low testosterone/IGF-1), unexplained weight changes and temperature sensitivity (thyroid dysfunction), and impaired recovery after workouts. Lab testing for hormone panels, sleep assessment, and inflammation markers can help identify specific dysfunctions.
Q: Are there safe clinical or supplement options to support repair hormones?
A: Non-prescription supports include optimizing diet, vitamin D, magnesium, zinc, omega-3s, and evidence-backed sleep aids like melatonin short-term. Prescription options (growth hormone, testosterone, thyroid replacement) should be used only under medical supervision for documented deficiencies because inappropriate use can create imbalance and side effects. Peptide therapies exist but require careful evaluation of safety and regulatory status. Always consult a clinician for testing and individualized treatment plans.
Q: How does timing of behaviors influence hormone-driven recovery?
A: Timing aligns hormone peaks with the body’s repair windows. Sleep onset triggers melatonin and growth hormone release, so consistent bedtimes and darkness are important. Protein intake spread through the day and post-exercise supports anabolic responses; resistance training earlier in the active phase may better engage anabolic hormones, while heavy exercise too close to bedtime can disrupt sleep. Fasting periods often boost autophagy at night when growth hormone is active. Synchronizing meals, exercise, and sleep with circadian patterns amplifies regenerative signaling.
Q: How do age and sex affect these repair signals, and what adjustments help across the lifespan?
A: With age, growth hormone, IGF-1, sex steroids, and melatonin decline, while inflammation tends to rise, slowing repair. Women and men have different baseline sex steroid profiles that influence muscle, bone, and immune responses; menopause and andropause shift those dynamics. Strategies that help older adults include resistance training, adequate protein (1.0-1.6 g/kg depending on needs), vitamin D and calcium for bone health, sleep optimization, targeted hormone replacement only when clinically indicated, and anti-inflammatory dietary patterns. Personalized plans that consider age, sex, comorbidities, and medications best restore balanced regenerative signaling.